Palliative care is an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment and treatment of pain and other problems, whether physical, psychosocial or spiritual.
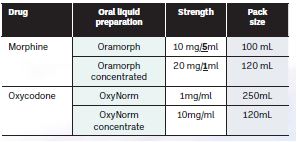
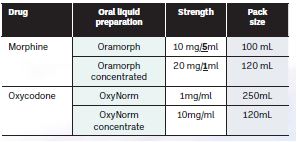
Opioids are commonly used in palliative care. They may be prescribed for a variety of indications. This article discusses the use specifically of oral liquid formulations of morphine (Oramorph) and oxycodone (Oxynorm). Morphine and oxycodone are usually prescribed for either pain or breathlessness. Methadone prescribing and usage differs significantly and is not discussed here.
With the exception of the lower strength of Oramorph, these preparations are included in Schedule 2 of the Misuse of Drugs Act. They are subject to controlled drug prescription writing, safe custody, record keeping and dispensing regulations.
Table 1: Oral liquid opioid preparations
Why use liquids?
- For small doses;
- For patients who find swallowing tablets difficult; and
- For patients with enteral feeding tubes.
Calculating an as required (PRN) dose
Where a patient is taking a regular opioid and using morphine or oxycodone as required (PRN) for breakthrough pain, the breakthrough dose should be proportionate to the background opioid dose. The national guideline for Pharmacological Management of Cancer Pain in Adults recommends dosing breakthrough opioids as either:
- 1/6 of the total 24-hour dose (commonly used in palliative care services); or
- 10-20 per cent of the total 24-hour dose.
It is recommended that doses falling outside of this range are queried with the prescriber.
Some patients may be using different opioids for background and breakthrough doses, for example a transdermal fentanyl patch for background with oral morphine for breakthroughs. In these cases, the appropriate breakthrough dose may not be immediately obvious, but opioid conversion ratios can be used to calculate the equivalent dose over 24 hours. The opioid conversion ratios used at Our Lady’s Hospice and Care Services are available on the Palliative Meds Info website (see olh.ie > Health & Social Care Professionals > Palliative Meds Info).
Note that potency is different if receiving medicines subcutaneously (by ‘syringe driver’).
Example: Patient is using a 12 micrograms/hour fentanyl transdermal patch every three days. What would be a suitable breakthrough dose of oral morphine?
|
Calculation |
Result |
| Calculate total fentanyl dose over 24 hours |
12 micrograms/hour
x 24 hours |
= 288 micrograms fentanyl over 24 hours |
| Convert micrograms to mg |
÷ 1000 |
0.288 mg |
| Convert from transdermal fentanyl to oral morphine* |
x 100 |
28.8 mg oral morphine equivalent over 24 hours. |
| Calculate a breakthrough dose (1/6 of total daily dose) |
÷ 6 |
4.8 mg |
| In practical terms, this dose will be rounded to the nearest conveniently measurable dose |
*Using the opioid conversion chart as referenced above, the ratio of transdermal fentanyl to oral morphine is 1:100.
Risk of error: Opioids are identified as high-risk or high-alert medicines by various institutions including the Health Information and Quality Authority and the Institute for Safe Medication Practices.
Medication errors
Medication errors, which have affected patients with palliative care needs using oral liquid opioids in the inpatient and community settings in Ireland, are described below. Details have not been given for anonymity, but these examples represent real incidents which have occurred, and have in some cases resulted in patient harm and/or admission to hospital or hospice.
Wrong drug
Problem: The wrong oral liquid opioid medicine is prescribed, dispensed or administered to the patient. As Oramorph and Oxynorm sound alike, this mistake can be easy to make. As the drugs have different potencies, if the patient receives the incorrect drug, they will be under- or over-dosed.
Solutions:
- Always read prescriptions carefully and ensure safe checking procedures are in place;
- Query/clarify changes from one opioid to another. This may be intentional as opioid rotation is common in palliative care, but the patient and healthcare staff involved should be able to confirm; and
- Does this prescription make sense with the background opioid? For example, a patient on Oxycontin regularly would not normally be prescribed Oramorph liquid for breakthroughs.
Wrong strength
Problem: The incorrect strength of oral liquid opioid is prescribed, dispensed or administered. As there is a 10-fold difference in strength between the ‘regular’ and ‘concentrated’ products for both morphine and oxycodone, this error can be fatal.
Solutions:
- Always read prescriptions carefully and ensure safe checking procedures are in place;
- Familiarise yourself with the appearance of these products to avoid confusion;
- Confirm that the dose necessitates prescribing/dispensing of the higher strength product; and
- If the patient is switched from lower to higher strength, for example, due to increasing dose, ensure they are aware of the change and the much smaller volume they will be using.
Mg or ml?
Problem: There is confusion about the dose of oral liquid opioid due to the dose or volume being referred to unclearly or inconsistently. This is particularly an issue for Oramorph 10mg/5mL, as this is a 2mg/mL solution, for example, if a patient is told to take 2.5mg but understands this as 2.5mL, they make inadvertently take double the intended dose.
Solutions:
- Consider adding the dose and volume to all oral liquid opioid instruction labels, for example ‘take 5mg (2.5mL) by mouth . . . ’;
- Show the patient or carer where to draw-up the dose to on the oral syringe. A label to mark the line may be useful;
- Be aware that patients may say ‘mill’ to refer to either mg or mL, and seek clarification if needed;
- Take extra care with patients/carers with limited literacy or poor vision; and
- Request clarification for prescriptions that don’t specify a dose clearly or give the dose only as a volume, the dose should always be prescribed in milligrams.
Incorrect dosing instructions
Problem: The patient has been advised verbally by their doctor or nurse to increase or decrease their dose of the oral liquid opioid, but this dose change is not communicated to the pharmacist nor is there an updated prescription provided.
The pharmacist continues to dispense and label the medicine based on the initial dose prescribed. The correct advice on how to measure the new dose may not be given to the patient and an appropriately sized oral syringe for measurement of the dose may not be supplied. There is a risk the patient will follow the outdated dosing information on the label.
Solutions: It is essential to ensure all dose changes are communicated between the pharmacist, the palliative care team and the GP and prescriptions are updated accordingly. A pharmacist could check with the patient/carer if the dose has been changed recently.
Incorrect dose administered
Problem: The patient or their carer is not clear on how to measure the dose and administers an overdose, resulting in toxicity (an underdose resulting in inadequate pain control is also possible).
Solutions:
- Always use oral syringes, not measuring cups;
- If the patient is taking multiple oral liquid medicines, ensure they are clear on which one is their painkiller and how to administer it. As the volumes can be small, assure the patient that this is the appropriate dose (patients may be used to taking higher volumes measured in spoons or measuring cups with other liquid medicines);
- Show the patient or carer where to draw up the dose to on the oral syringe. A label to mark the line may be useful; and
- Do not assume someone else has discussed with the patient/carer when there has been a change in dose or product.
Injection of oral medicines
Problem: Oral liquid opioids prepared in unsuitable syringes can be administered via the patient’s intravenous or subcutaneous line. This can result in tissue damage and can be fatal.
Solutions:
- Check the patient’s understanding of how to administer their oral liquid medicines;
- Only use labelled oral/enteral syringes that cannot be connected to intravenous catheters or ports to measure and administer oral liquid medicines;
- Never use intravenous syringes to measure and administer oral liquid medicines. Administration of medication via the wrong route is considered a Never Event by the NHS (Recommendations from National Patient Safety Agency alerts that remain relevant to the Never Events list 2018, available at nhs.uk). The UK National Patient safety Alert issued in 2007 remains relevant (Patient Safety Alert 19. Promoting safer measurement and administration of liquid medicines via oral and other enteral routes);
- For patients with an enteral feeding tube, medicines should only be administered using ENFit syringes (compatible with ISO 80369-3). Bottle adaptors that fit ENFit syringes are available; and
- Consider adding ‘by mouth’ (or by PEG tube etc.) to all oral liquid opioid instruction labels.
Is it regular or PRN?
For patients who cannot take a modified release tablet such as MST Continus or Oxycontin, they may be prescribed an oral liquid opioid regularly, for example every six hours. They may also then have the option to take breakthrough doses in between the regular doses. It is important that the patient understands to take the regular doses ‘by the clock’, and that they know when to take the breakthrough doses, and what the minimum interval should be between doses.

Patient education is essential
On each occasion that the oral liquid medicine is prescribed, dose adjusted or dispensed, advising the patient or their carer or family member who administers their medicines on how to measure the prescribed dose of the oral liquid opioid medicine using an appropriate oral syringe is essential to the safe use of these medicines. The pharmacist dispensing the medicine can demonstrate how the correct dose should be drawn into the oral syringe. There is a shared responsibility between the prescriber, the discharging hospital/hospice team, the community pharmacist and the community palliative care team members to carry out this education and check the patient’s understanding of how to administer the correct dose of their medicine.
References available on request.
Further information
For further information, please visit the Palliative Meds Info webpages (
olh.ie > Health & Social Care Professionals >
Palliative Meds Info), where the following documents as well as other resources about opioids are available:
- The Use of Oral Morphine Sulphate in Palliative Care;
- Oramorph for breathlessness: Patient Information Leaflet; and
- Opioid Conversion Chart.