Home » Urinary tract infection in older people
In this article, Mala Shah, Chief II Antimicrobial Pharmacist, National Quality and Patient Safety Office, HSE Community Healthcare, discusses some key practice points for pharmacists for the assessment and management of suspected urinary tract infection (UTI) in older adults (age 65years and over).
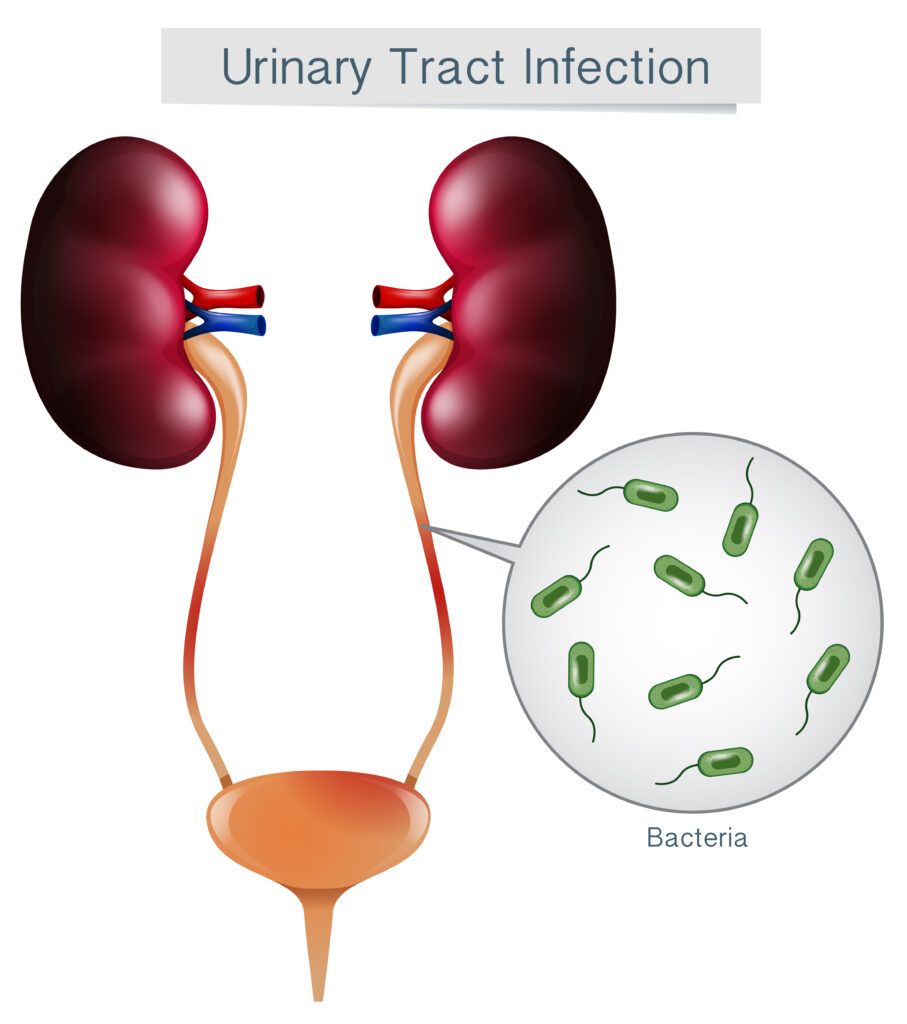
A urinary tract infection (UTI) develops when bacteria enter the bladder through the urethra and multiply, causing tissue damage and disease in the urinary tract. UTIs are usually caused by bacteria that live in the bowel. The most common pathogen causing UTI is E. coli.
Urinary tract infections are common bacterial infections in older adults. Older adults are more likely to have conditions that predispose them to infections in general (for example, age-associated changes in immune function, diabetes, stroke, dementia) and UTI in particular (for example, faecal impaction, bowel or bladder incontinence, high urinary residual volumes and long-term indwelling catheters).
The HSE Older Persons RCFs Antimicrobial PPS 2020/21 reported that UTIs accounted for 50% of infections treated with antibiotics. Studies have found a higher prevalence of overall antibiotic use and prophylactic antibiotic use in residential care facilities in Ireland compared to European mean.
Pharmacists have an important role to play in antimicrobial stewardship (AMS) for UTI, along with other healthcare professionals.
Antimicrobial resistance (AMR) among urinary pathogens is increasingly common. Key modifiable risk factors of AMR in UTIs are the overuse of broad-spectrum antimicrobials (for example, co-amoxiclav and quinolones), unnecessarily prolonged durations of treatment, and unnecessary use of antimicrobials when they are not indicated.
The Urinary Tract Infection Information for people over 65 years is a patient leaflet for UTI in older adults. Community pharmacists can use this tool when counselling patients on the management of UTI. This leaflet is available at antibioticprescribing.ie > Antimicrobial use in Residential Care Facilities and Nursing Homes > Skip the Dip for UTI in over 65s campaign.
Pharmacists are well-placed to advise patients of preventative measures:
Pharmacists should be aware of the key signs and symptoms of UTI and refer patient to their doctor as appropriate. It is worth remembering that in the absence of clinical signs and symptoms, dark and/ or foul smelling urine are not usually suggestive of a UTI, and may be a sign of dehydration.
Signs and symptoms of UTI in older adults are:
(*Acute confusion in the elderly can be caused by urinary infection, but other causes should also be considered, including pain, change in environment, side effects of medicines, other infection, poor sleep, hydration, diet and constipation.).
“ It is worth remembering that in the absence of clinical signs and symptoms, dark and/ or foul smelling urine are not usually suggestive of a UTI, and may be a sign of dehydration.”
Pyelonephritis / upper urinary tract infection (UTI) should be considered when there is:
Pyelonephritis and suspected sepsis requires prompt medical assessment.
Pharmacists should be aware that dipstick urinalysis is not recommended for assessment of evidence of UTI in older adults (age 65 years and over).
Some questions to consider:
Often, treatment is empiric unless recent urine culture results are available with antibiotic sensitivities to guide the choice of agent.
Refer to the considerations with antibiotics commonly used for UTI section for useful information for individual antibiotics.
AMR among urinary pathogens is increasingly common and resistance to first line agents is a concern. For older people in RCFs where AMR is more prevalent, it is advised that a urine sample is sent to the laboratory for culture and sensitivity testing for all suspected UTI. The results should be used to guide or modify empiric treatment choices as necessary.
The duration of treatment for UTI in community settings varies depending on type of UTI:
In certain circumstances, for proven recurrent UTI, a trial of antibiotic prophylaxis may be appropriate if non-antimicrobial measures are unsuccessful.
The adverse effects of antibiotic prophylaxis should be considered and discussed with the patient. These include:
All UTI antimicrobial prophylaxis should be reviewed after three to six months with a view to de-prescribing. There is limited evidence of any additional benefit from such prophylaxis beyond three to six months. Prolonged use of antibiotic prophylaxis will increase the likelihood of adverse effects and antimicrobial resistance, which decreases future treatment options for the patient.
Discuss de-prescribing UTI prophylaxis with prescriber if the answer is yes to any of the following questions:
An audit tool to aid regular review of patients receiving antimicrobial urinary prophylaxis is available on antibioticprescribing.ie > Antimicrobial Stewardship > AMS Resources and Audit Tools.
There is limited evidence for other preventative measures including cranberry products, D-mannose, methenamine hippurate and probiotics.
Nitrofurantoin is a Green antibiotic and the preferred first choice agent for uncomplicated UTI. Nitrofurantoin resistance rates remain low in community E.coli UTIs throughout Ireland (including in ESBL-producing isolates) despite increasing resistance to other antibiotics. In addition, it is a narrow spectrum agent with less likelihood of collateral damage to the gut and development of AMR.
Some practice points for nitrofurantoin:
This is a Green (preferred) antibiotic. Not to be used if history of anaphylaxis with penicillin.
Recommended dose depends on indication:
This is a Green (preferred) antibiotic for UTI. However, in older people in RCFs, there is data to indicate that the rate of trimethoprim resistance in E. coli is high in this population. Empiric trimethoprim is therefore no longer recommended except where nitrofurantoin is unsuitable and the risk of resistance is low (for example, where a recent urine culture has had a trimethoprim-susceptible isolate and trimethoprim has not been used, or in a young patient without a significant antibiotic exposure history).
Although it is a Green (preferred) antibiotic for respiratory tract infection, it is not a first line agent for empiric treatment of UTI as resistance rates in community E. coli UTIs are extremely high. Amoxicillin should only be used if susceptibility is known.
It is a Red (non-preferred) antibiotic for UTI. Resistance to co-amoxiclav in E. coli in community urine samples is high. In addition, it is a systemic agent and should be avoided in uncomplicated cystitis if a locally acting agent (for example, nitrofurantoin) could be used instead.
This is a Red (non-preferred) antibiotic. It is a broad-spectrum antibiotic, associated with C. difficile infection and severe and long-lasting adverse effects involving the muscular, nervous and cardiovascular systems.
Patients need to be informed of the potential adverse effects of ciprofloxacin, balanced with its role in the treatment of infection.
It is not recommended for the empiric treatment of uncomplicated cystitis where other antibiotic treatment options are available.
It is not recommended for UTI prophylaxis.
It may be considered for targeted therapy of multi-resistant infections, where there are no other appropriate antibiotics for the patient.
Refer to the fluoroquinolone warning on antibioticprescribing.ie for more information (> Drug Interactions).
Fosfomycin is a Green (preferred) antibiotic. To preserve the efficacy of this drug, its use should be limited to second-line treatment. Many multi-resistant community UTI isolates (including ESBL-producing E. coli) remain susceptible to fosfomycin. Fosfomycin is not recommended in patients with creatinine clearance <10 mL/min.
It should be taken on an empty stomach, preferably before bedtime and after emptying the bladder. The dose should be dissolved into a glass of water and taken immediately after its preparation.
Skip the Dip for UTI in over 65s initiative
Dipstick urine testing is an engrained practice for many healthcare professionals as part of routine assessment of patients. However, dipstick urine testing can lead to unnecessary antibiotic use for UTI in older people, and it is no longer recommended for the assessment of evidence of UTI in older adults (65 years and over).
Markers that may indicate UTI on urine test strips include leucocyte esterase and nitrites. However, the detection of leucocyte esterase and/or nitrites in urine dipstick tests is not a reliable method for assessing for evidence of UTI, especially in older adults because of the high prevalence of asymptomatic bacteriuria in older adults.
Asymptomatic bacteriuria (ASB) is the presence of bacteria in the urine without symptoms of a UTI. It can be present at any age but is particularly common in those aged over 65 years (up to 50% people <65 years have ASB) and it is very common in those persons with an indwelling urinary catheter (100% have ASB after catheter in situ for >30 days). Urine dipstick tests are not a useful tool to assess for evidence of UTI in older people as they do not distinguish between ASB and UTI. ASB can lead to positive results for markers of UTI in urine dipstick tests, even in those without a UTI. Inappropriate use of dipstick urinalysis can lead to unnecessary antibiotic prescribing which does not benefit the patient and may cause considerable harm including adverse effects, drug interactions, and antimicrobial resistance.
Skip the Dip for UTI in over 65s is a quality improvement initiative in HSE Older Persons Residential Care Facilities (RCFs) led by HSE Community Antimicrobial Pharmacists and the HSE Quality and Patient Safety Office, in collaboration with the national AMRIC team. Commencing in September 2023, this new initiative aims to reduce the levels of inappropriate prescribing for urinary tract infections (UTIs) in people aged 65 years and older. Further information is available in the Antimicrobial use in Residential Care Facilities including Nursing Homes section of antibitoicprescribing.ie.
A recent study from Australia reported reduction in antibiotic use after implementation of a similar initiative in older person RCFs.
Mala Shah

Chief II Antimicrobial Pharmacist, National Quality and Patient Safety Office, HSE Community Healthcare
Highlighted Articles