Home » Update on Management of Acute Pain in Community Pharmacy

By the end of this article, you should be able to:
Acute pain is recent-onset, short-term pain (usually up to three months), that signals actual or potential tissue damage and resolves as the underlying cause heals (US Pain Foundation). First-line treatment depends on pain type and individual factors, including clinical presentation, comorbidities, and contraindications. Following a stepwise approach, in-line with the WHO pain ladder, acute pain management starts with simple analgesics, escalating only after careful assessment. Dosing should be individualised, balancing therapeutic benefit against potential side effects, matching treatment to pain type and severity. NICE CKS advises avoiding combination analgesics initially, allowing flexible dose adjustment. Pharmacists should review the SPCs and counsel patients on dosing, side effects, and the importance of reading the patient information leaflet. Common conditions in the community include dental pain, low back pain, headaches, and period pain.
Dental pain can be difficult to distinguish from other types of pain and usually requires assessment by a dentist. Signs include unilateral mouth pain, spontaneous or nocturnal pain and pain triggered by chewing or hot/cold and sweet/acidic foods. Dental pain can be intense and typically requires pain relief. The choice of analgesic should consider individual risks and contraindications, with ibuprofen and/or paracetamol being appropriate first-line options in most cases (HSE) (see Table 1).
Low back pain (LBP) is the most prevalent musculoskeletal condition globally, with most people experiencing it at least once during their lifetime (WHO, 2023). Acute LBP lasts less than six weeks and may present as dull or sharp pain, sometimes radiating to the legs, affecting movement, daily activities, sleep, and mood. First-line management includes physical therapy, lifestyle modification, and reducing strain; with medicines used as adjuncts to support symptom relief (WHO, 2023).
Dysmenorrhoea (period pain) is cramping pain experienced in the lower abdomen before or during menstruation. It can range from mild discomfort to severe pain and may also affect the lower back and thighs. Dysmenorrhoea may occur with normal menstrual cycles (primary) or be caused by an underlying condition such as endometriosis or fibroids (secondary). First-line treatment includes ibuprofen and/or paracetamol to relieve pain, along with lifestyle measures such as gentle exercise, heat therapy (for example, a hot water bottle) and relaxation techniques (NHS).
Headaches are a common presentation in community pharmacy, ranging from mild to severe, with tension-type headaches and migraines most frequently seen. First-line treatment includes paracetamol or an NSAID, alongside advice on rest, hydration, and stress management. Aspirin may be considered for the treatment of tension-type headaches. Referral is recommended if symptoms are severe, persistent, or atypical (NICE, HSE).
Table 1: Common acute pain conditions and recommended evidence-based OTC analgesics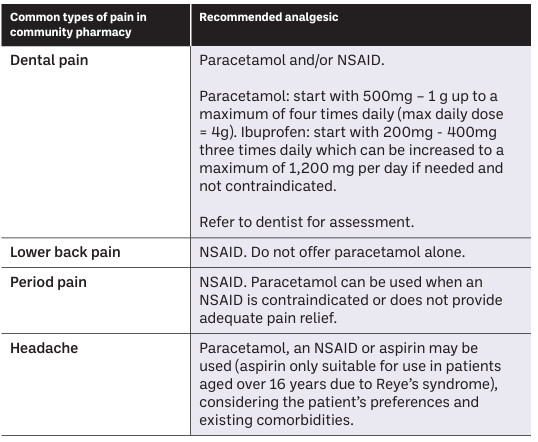 Source: NICE, HSE
Paracetamol
Paracetamol is an appropriate first-line option for mild to moderate acute pain. Although it lacks anti-inflammatory effects, it has no significant GI, renal, or cardiac adverse effects at standard doses. To reduce the risk of overdose, pharmacists and OTC assistants should check the use of other prescribed or OTC products containing paracetamol (see Scenario 1).
Source: NICE, HSE
Paracetamol
Paracetamol is an appropriate first-line option for mild to moderate acute pain. Although it lacks anti-inflammatory effects, it has no significant GI, renal, or cardiac adverse effects at standard doses. To reduce the risk of overdose, pharmacists and OTC assistants should check the use of other prescribed or OTC products containing paracetamol (see Scenario 1).
A 41-year-old man presents to your pharmacy and asks your OTC assistant for two packets of paracetamol. When the assistant informs him that he can only purchase one box per sale, he replies:
“I’m not going to overdose on paracetamol, am I?”
OTC assistant actions and consultation |
| Your experienced OTC assistant can handle the consultation as follows. |
| Sample dialogue: |
| “Paracetamol is included in many cold, flu and sinus remedies as well as standard painkillers, so people can sometimes take more than the recommended amount without realising.” “It is the drug most frequently involved in both intentional and accidental overdoses in Ireland” (gov.ie, NSHRI). “It is generally safe at recommended doses, but taking more than the maximum adult daily dose can overwhelm the liver and cause serious damage” (HPRA). |
| The OTC assistant can clearly explain the adult dosing: 500 mg–1 g per dose (depending on formulation), not exceeding 4 g in 24 hours, with appropriate spacing between doses, and check whether the patient is taking any other medicines containing paracetamol. They provide clear examples of combination products available for sale, including analgesics, cold, flu and sinus remedies and explain why pack-size limits exist as a harm-minimisation measure in Ireland. Reducing the quantity available per transaction has been shown to help decrease overdoses and related harm (gov.ie). |
Patient perspective and outcome |
| The patient responds that he hadn’t realised how many everyday OTC products contain paracetamol and had always assumed it was harmless. After the consultation, he states that the information about liver risk with overdose was new to him and that he now plans to check labels and patient information leaflets more carefully and only take the recommended doses. He expresses appreciation for the OTC assistant’s calm, informative approach. |
Non-steroidal anti-inflammatory drugs (NSAIDs) Ibuprofen is the preferred first-line NSAID for many types of pain, including LBP, period pain, and toothache. Contraindications include active gastrointestinal bleeding or ulceration, history of NSAID-related GI bleeding, or recurrent ulcers, hypersensitivity to NSAIDs or allergic reactions causing asthma, rhinitis, angioedema, or urticarial and severe heart failure, liver impairment, or kidney impairment. Caution is needed in older adults, those with comorbidities, patients taking interacting medications, or those at higher risk of GI or cardiovascular side effects (see Scenario 2).
Scenario 2: Frequent requests for OTC NSAIDs should prompt a clinical review of symptom patterns and medicine use
A 32-year-old woman presents to your pharmacy requesting ibuprofen for migraine relief. Your OTC assistant informs you that this patient has been purchasing NSAID-containing products frequently.
| Pharmacist actions and consultation |
| The pharmacist invites the patient to a private consultation area and uses open-ended, non-judgmental questions to explore her symptoms and medicine use. |
| Sample dialogue: |
| “Can you tell me a bit more about how often you’ve been getting these headaches and how frequently you’re using ibuprofen?” “Ibuprofen can be very effective for short-term pain, but when it’s used regularly over a long period, it can increase the risk of side-effects, including stomach irritation and kidney problems” (SPC). “Because you need pain relief quite often, it might be worth having a GP review to confirm whether these are migraines and to discuss safer long-term management options.” |
| The pharmacist explains appropriate dosing limits and advises against ongoing frequent NSAID use without medical supervision. |
| Patient perspective and outcome |
| The patient states that she was unaware of the potential long-term risks associated with regular NSAID use and had never received a formal diagnosis of migraine. She expresses appreciation for the information provided and agrees that a review with her GP would be beneficial. She leaves the pharmacy feeling informed, reassured, and supported in seeking further medical assessment. |
Codeine
Codeine is not an appropriate first-line analgesic choice and should only be used in combination with first-line analgesics (paracetamol or NSAIDs) within a combination product for acute pain, if first-line analgesics are ineffective. The need for access to opioids must be balanced with concerns about the harm arising from the misuse of these medications in pain management (WHO). Codeine is contraindicated in patients with respiratory depression, severe asthma, paralytic ileus, or hypersensitivity. Caution is needed in the elderly, those with liver or kidney impairment, or a history of substance misuse. Codeine–paracetamol may be used for acute LBP if an NSAID is contraindicated, not tolerated, or ineffective, but opioids should not be used for tension-type headaches or migraines (NICE). PSI guidance states that codeine products must not be available for self-selection and can only be supplied under pharmacist supervision and used for the shortest duration (no more than three days). The maximum OTC doses are typically eight tablets of codeine 8 mg/paracetamol 500 mg or six tablets of codeine 12.8 mg/ibuprofen 200 mg in 24 hours. Pharmacists must counsel patients on proper use and the risks of tolerance and dependence (see Scenario 3).
Scenario 3:
A 46-year-old woman presents to your pharmacy requesting a second line paracetamol- codeine combination product for a headache. An OTC medicines assistant begins asking the PSI required screening questions.
The patient interrupts impatiently:
“I need something quick that will work fast — I don’t have time to wait!”
Pharmacist/assistant consultation |
| The assistant responds calmly and explains the rationale for codeine restrictions and safety considerations. The patient is referred to the pharmacist who continues the screening questions and uses open-ended questions to assess the headache. |
| Sample dialogue: |
| “I understand you need quick relief. However, we usually recommend trying other options first to see if they provide sufficient relief, before we consider second-line combination analgesics containing codeine as we want to avoid potential side effects like drowsiness or constipation. Can I ask how severe your headaches are and what you normally take for them?” |
| “Paracetamol is an excellent first-line analgesic, for faster relief, some patients choose products containing paracetamol with caffeine, as the caffeine helps the paracetamol work more quickly, and it avoids the unwanted side effects associated with codeine.” |
| The pharmacist explains appropriate dosing for adults, including maximum daily limits and spacing, and asks about any other medications or health conditions. They reassure the patient that this approach is effective and safe, while noting that codeine-containing products are available under supervision if first-line options are ineffective. |
Patient perspective and outcome |
| The patient appreciates the advice on faster-acting, safer alternatives to codeine and feels reassured that she can manage her headache effectively without unnecessary opioid use. She leaves the pharmacy feeling informed and confident in the recommended treatment. |
Community pharmacists play a pivotal role in the safe and effective management of acute pain, supported by thorough, patient-centred consultations. By applying a structured, stepwise approach, pharmacists and their teams can tailor analgesic recommendations to individual patient needs while minimising the risk of harm. Providing clear information and advice empowers patients to use pain relief safely and effectively, supporting optimal outcomes and reinforcing the pharmacist’s role as a trusted healthcare professional.

Highlighted Articles