Home » The Medication Safety Minute
A team comprising Dr Eileen Relihan and two medical consultants in St James’s Hospital, Dr Finbarr O’Connell and Dr Una Kennedy, developed an innovative approach to sharing learning in relation to medication safety issues in the hospital — a project called the Medication Safety Minute. The project involves the design and delivery of bite-sized weekly, medication safety messages (‘Minutes’) to prescribers, which take just one minute to review. This article provides an overview of the project.

The Medication Safety Minute initiative was introduced in 2017 and to date over 150 ‘Minutes’ have been published, highlighting prescribing risks and measures to minimise potential patient harm. The messages are designed for St James’s Hospital (SJH), but since its inception the project has stimulated interest amongst healthcare professionals at a national and international level. At the present time, the ‘Minutes’ are used in some capacity by the majority of hospitals in Ireland, they are distributed to hundreds of GPs and community pharmacists each week and are incorporated into both undergraduate and postgraduate teaching in TCD and the Royal College of Physicians, Ireland.
Dr Relihan explains how the programme was established and its impact on medication safety in SJH, over the following questions.
A significant aspect of any medication safety programme is the dissemination of learning regarding risks to healthcare staff. However, access to and engagement with doctors has traditionally been very challenging in the hospital environment where there are multiple competing priorities and information overload. The long-standing system of emailing detailed medication safety bulletins to doctors had had limited success, with anecdotal evidence suggesting that many clinicians did not access the information due to time constraints and work pressures. Our aim was to design safety messages in a novel format which, enabled the content to be assimilated in one minute or less.
We based the design of the Medication Safety Minute on the concept of microlearning, which is a mode of teaching involving the delivery of focused nuggets of information over very brief time periods. There is evidence that splitting learning up into small, manageable chunks makes information easier to understand and remember compared to lengthy teaching sessions which can overload recipients.
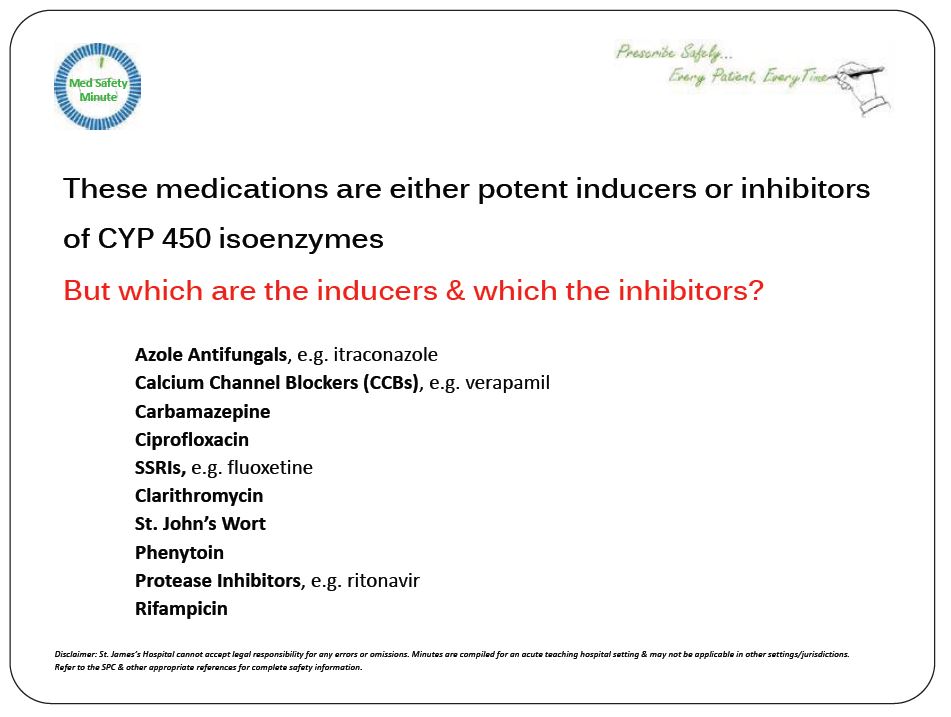
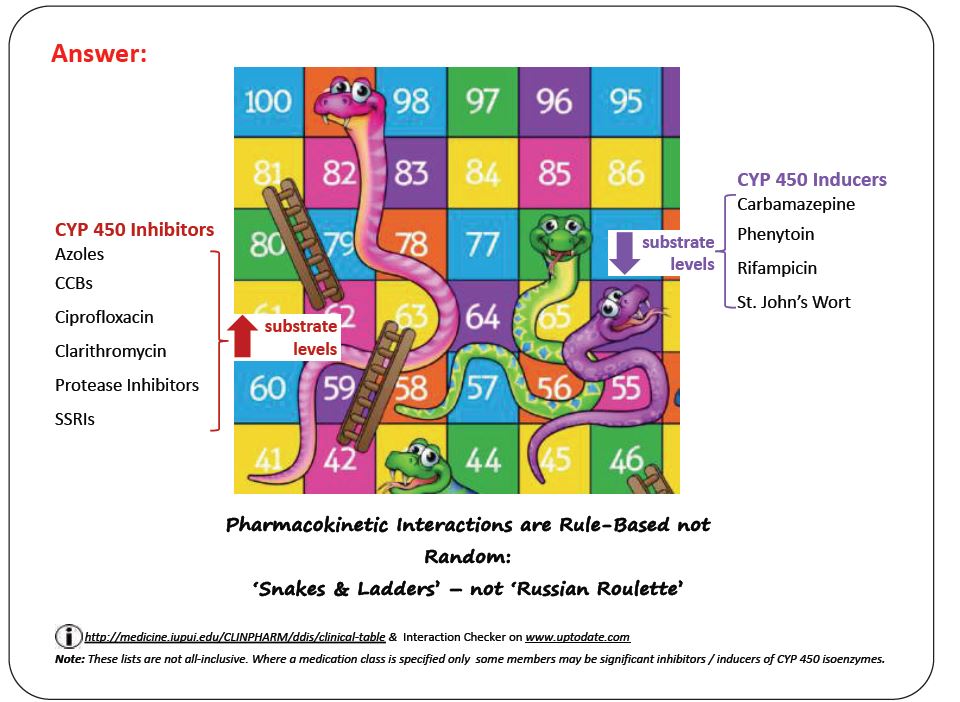
We designed the message format to optimise engagement with prescribers by using a question and answer configuration and employed ‘visual language’ (i.e. minimal text with graphics used instead where possible), to optimise understanding and retention of the information. We availed of all possible modes and channels of communication to reach our target audience, for example email, an intranet home page banner, a weekly PowerPoint display at Grand Rounds, intern teaching sessions and medical update meetings. In addition, we adopted less conventional dissemination strategies, i.e. WhatsApp, to message doctors on their mobile phones as well as social media.
With every ‘Minute’ there is a challenge in balancing brevity with functionality — one needs to curate text and graphics to fit the constraints of a very concise format whilst ensuring that the message being delivered is unambiguous and adding value. This can only be achieved by an iterative process of review in collaboration with the clinicians in the specialist area, and repeatedly reworking the material until optimal.
Another challenge is the resources required to produce quality content on a weekly basis. In the initial months of the project, we generated a new Medication Safety Minute every week. However, to make the workload more sustainable, we then switched to a more manageable schedule where we alternate a new publication with previously issued ‘Minutes’ from the archive.
I think having two senior consultants on the project team was critical to the success of the initiative as it help garner the support of front-line prescribers. In addition, strong working relationships with clinicians across the medical and surgical specialties were essential, as these were the staff who assisted in reviewing the material and promoting the messages to their teams.
I would also advise being realistic about the effort required to sustain a project like this over the long-term — it is considerable — so I would recommend carefully considering the publication schedule your team can commit to.
Our goal has been to issue safety messages which are of genuine value to prescribers without burdening them with of large volumes of data. The appeal of the ‘Minute’ is that it extracts the key safety issues in the pharmacological management of a condition that we know is high risk. This information is drawn from frontline experience and not typically taught in universities or readily available in textbooks, and it resonates with healthcare staff because it involves observations from ‘real-world’ practice. Over time consultants in the hospital have come to appreciate these features of the ‘Minute’ and use it as a teaching tool with their teams on ward round and in education sessions.
Yes of course. The ‘Minute’ is a teaching tool and as such its influence is limited because staff education, although essential, is the intervention known to have the least impact on safety. The approach I apply in relation to minimising risk and error is based on the concept of a hierarchy of hazard control which stratifies risk controls according to their effectiveness.
According to this framework, one should first aim to eliminate the risk (for example by removing a high risk medication from general ward areas, which don’t require it in order to reduce the risk of a selection error at administration), but if this is not possible then the idea is to move to the next most robust response in the hierarchy (for example, introducing forcing functions in an e-prescribing system), and so on, until one reaches the most robust intervention possible that can feasibly be implemented. Sometimes multiple interventions combined from different levels in the hierarchy are the optimal way to target a safety concern. Education and training are at the bottom of the hierarchy in terms of effectiveness, but nevertheless are almost always an essential component of the response to minimising risk.
Medication safety issues are inevitable in hospitals, but our goal is to take steps to minimise risk as far upstream in the process as possible (before an actual error arises) and — in the event of an error occurring — to optimise the response to prevent or minimise the possibility of patient harm. In order to do this, one first needs to acquire a comprehensive understanding of the safety status of the organisation by accessing multiple sources of data — both formal and informal — from both within and outside the organisation (for example, audits, error reports, surveys, complaints, claims, published literature, conversations with colleagues, safety culture measurements). This data is then used to inform the design of safety solutions which are embedded in systems to make it as easy as possible for staff to use medication safely.
It is critical. In an acute teaching hospital, the medication use process involves several professions — pharmacists, doctors and nurses — with varying levels of experience and seniority, working in a myriad of roles across multiple specialities. It is so important that a positive safety culture is fostered in the organisation so that any staff member, regardless of position or rank, feels supported to highlight a risk and then that the focus is on shared learning and collaboration between disciples to develop safety solutions.
I think the overriding challenge facing pharmacists, currently relates to automation technology which is rapidly evolving the healthcare landscape, for example, robotics, artificial intelligence, automated dispensing systems and cabinets, electronic pharmacy management systems, point-of care testing. These innovations have tremendous potential to improve patient care and reduce costs but can also introduce new risks — some of which can be predicted and mitigated against — but likely also some issues which are unforeseeable. For example, in SJH our experience with an e-prescribing system has been that its introduction in 2018 was only the first step of the journey, because it is the programme of ongoing evaluation, maintenance and configuration of the system, which ensures that the technology continues to deliver the intended benefits including enhanced patient safety.
The Medication Safety Minutes can be accessed on the social media platform X (@medsafetymin); via an electronic flipbook, which is a free open-access resource (available at heyzine.com/flip-book/9ef7b6a49b.html); or by subscribing to a weekly email publication — email erelihan@stjames.ie to subscribe.
Dr Eileen Relihan MPSI is the Medication Safety Facilitator at St James’s Hospital (SJH), Dublin, Ireland, a position which involves management of the medication safety programme in the organisation. She is also an Adjunct Clinical Fellow for the School of Pharmacy, Trinity College Dublin (TCD) and lectures at both undergraduate and postgraduate level for the TCD Schools of Pharmacy, Medicine and Nursing.
Examples of Medication Safety Minutes
Dr Eileen Relihan

Medication Safety Facilitator, St James’s Hospital (SJH)
Highlighted Articles