Home » Respiratory tract infections and antimicrobial stewardship

Respiratory tract infections (RTIs) are one of the most common reasons for presentation to community pharmacies and contribute to a substantial loss of productivity and absence from work and school.
The majority of RTIs are caused by viral pathogens (for example, rhinovirus, adenovirus, influenza, COVID-19 and RSV) and affect a large proportion of the population every year. Upper respiratory tract infections (URTIs) are particularly common among infants and children (up to 10 to 12 infections per year) but become less common as children mature. Many URTIs are self-limiting viral infections and antibiotics are usually not indicated. Certain RTIs, for example pneumonia, can cause severe morbidity and prompt antibiotic treatment is important.
Community pharmacists have a key role in reducing unnecessary antibiotic use, providing advice on self-management of symptoms with/without over the counter remedies and can provide advice on measures to prevent onward transmission. Informing people how long it takes to get better from infections can help to manage their expectations (see Table 1). Community pharmacists are also in unique position to provide triage for those that may require a doctor’s consultation or emergency department referral.
Table 1: Time taken to get better from some common RTIs
| Infection: | Most are better by: |
| Sore throat | 7 days |
| Sinusitis | 14 – 21 days |
| Common cold | 14 days |
| Cough or bronchitis | 21 days |
We will give a brief overview of some common RTIs, identifying the role a community pharmacist can play in managing symptoms and in supporting antimicrobial stewardship. Guidance for RTIs can be found on antibioticprescribing.ie.
Table 2: ‘What’s New’ on RTI guidelines — topic and date updated
| Acute cough/bronchitis: September 2024 The antibiotic treatment table has been removed to reflect international best practice. Acute cough/bronchitis is caused mainly by viruses and is a self-limiting condition. In the majority of cases, antibiotics are not indicated. |
| Sinusitis: September 2024 Addition of dosing table for intranasal steroids to be considered for people with symptoms of around 10 days or more. Note added regarding duration of treatment for severe/worsening infection. |
| Pharyngitis, sore throat and tonsillitis: September 2024 Note added that FeverPain tool has not been assessed in children under three years. Recommended dose of cefalexin for adults amended. |
| COPD: September 2024 Updates to expert advisory comments and removal of levofloxacin from the empiric treatment table. |
| Community Acquired Pneumonia (CAP): September 2024 Addition of information with advice on treatment of aspiration pneumonia. Recommended dose of amoxicillin amended. |
| Pneumonia in residential care facilities: September 2024 Updates to guidance on aspiration pneumonia. Some antibiotic dose amendments. |
Extract from ‘What’s New’ on antibioticprescribing.ie. This page, linked from the homepage on antibioticprescribing.ie, provides information on “whats new on antibiotic prescribing”, and flags recently updated content on the website.
Acute bronchitis is a self-limiting inflammation of the bronchi characterised by cough as the predominant symptom; and at least one other lower respiratory tract symptom, such as sputum production, wheezing, chest pain; and the absence of another explanation for the symptoms (for example, pneumonia, infective exacerbation of COPD). Viruses cause most cases of acute bronchitis in healthy adults and children and antibiotics are not usually indicated.
Pharmacists can advise on symptom control (see Table 3), rest and hydration and advise the patient that the acute cough may persist for up to three to four weeks. Patients may be unaware that yellow/green coloured sputum does not necessarily indicate bacterial infection or the need for antibiotics. Advise patient to seek medical attention if symptoms worsen rapidly or significantly, or they become systemically very unwell.
Table 3: Symptom control for acute cough/bronchitis
Consider other causes of cough, for example, asthma, COPD, pulmonary embolism, smoking, heartburn, hay fever. Refer patients for medical attention if they have a cough that doesn’t go away after three weeks, or they are coughing up blood, have persistent tiredness or breathlessness or unexplained weight loss.
Figure 1: Scarlet fever (scarlatina)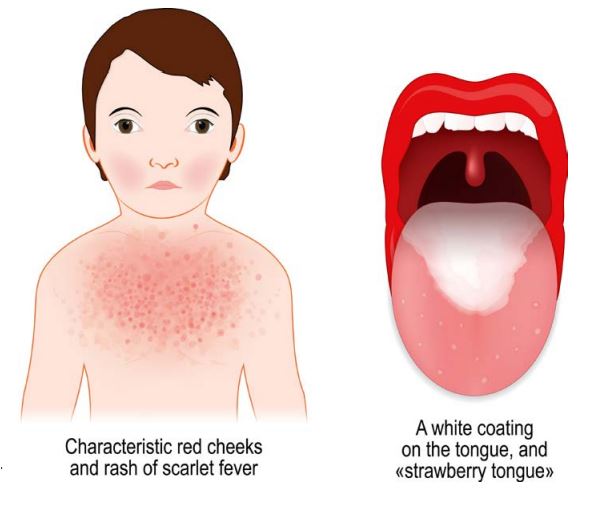
Acute sinusitis usually follows a common cold. Symptoms for 10 days or less are more likely to be associated with a cold rather than an acute sinusitis. Prolonged symptoms (10 days or more with no improvement), could be due to either viral or bacterial acute sinusitis. Bacterial sinusitis is usually self-limiting and does not routinely need antibiotics. 80 per cent of cases resolve in 14 days without antibiotics and offer only marginal benefit after day seven. Bacterial cause may be more likely if several of the following are present; symptoms for more than 10 days, discoloured or purulent nasal discharge, severe localised unilateral pain (particularly pain over teeth and jaw), fever or marked deterioration after an initial milder phase. If these symptoms are present, advise the patient to seek medical attention. Other red flags for referral to doctor include changes in vision, severe frontal headache or other neurological signs.
For symptom relief pharmacists can advise on the use of paracetamol (or ibuprofen where appropriate) for the treatment of pain or fever. There is little evidence of benefit, but patients may wish to try systemic decongestants, topical decongestants or saline preparations for local irrigation (for example, nasal rinses, sprays, drops).
Patients may present with a prescription for high dose intranasal steroids. Guidance for prescribers on the use of intranasal steroids for sinusitis is available on antibioticprescribing.ie. Pharmacists have an important role in advising on use of nasal sprays to alleviate symptoms.
Some patients may receive a delayed/back-up antibiotic prescription when the prescriber determines there is no immediate need for an antibiotic. Pharmacists can play a key role here in encouraging the patient to follow the prescriber’s instructions on if, and when, to fill the antibiotic prescription.
If an antibiotic is required, the recommended duration of treatment is five days in most cases. Refer to antibioticprescribing.ie for more details.
Clinical descriptions of acute sore throat include acute pharyngitis, inflammation of the part of the throat behind the soft palate (oropharynx); and tonsillitis, inflammation of the tonsils. The majority of sore throats are viral, and most patients do not benefit from antibiotics. Antibiotics make little difference to how long symptoms last or the number of people whose symptoms improve. Pharmacists can advise on the use of the following for symptom relief:
Acute sore throat caused by bacteria (mostly Streptococcus pyogenes also known as Group A Streptococcus) are uncommon. The most common complication is otitis media. Patients with severe symptoms or who are clinically unwell should be referred to a doctor.
Several clinical scoring systems have been developed to identify patients with higher likelihood of sore throat being caused by Streptococcus pyogenes. The FeverPAIN scoring system is an example of such a tool, see Table 4. The FeverPAIN scoring system helps to identify those who are most likely to benefit from antibiotics. This tool has not been assessed in children under three years.
Each of the FeverPain criteria score one point (maximum score of five). Higher scores suggest more severe symptoms and likely bacterial (streptococcal) cause; therefore the patient is more likely to benefit from antibiotics if they have a higher score.
Table 4: FeverPAIN scoring system for children >3 years old and adult
FeverPAIN criteria:
Where an antibiotic is deemed necessary, the recommended duration of treatment is five days. Depending on clinical response, duration can be extended to 10 days in total. If scarlet fever is suspected, it is advisable to treat for 10 days duration. Guidance on antibiotic use for sore throat is available on www.antibioticprescribing.ie.
A common presentation of Group A Streptococcus in children can be scarlet fever. The first signs of scarlet fever can be flu-like symptoms, including a high temperature, a sore throat and swollen neck glands (a large lump on the side of the neck). A rash appears 12 to 48 hours later. It looks like small, raised bumps and starts on the chest and tummy, then spreads. The rash makes skin feel rough, like sandpaper.
Community acquired pneumonia (CAP) is a pneumonia that is acquired outside of hospital. The defining characteristics of CAP include cough and at least one other lower respiratory tract symptom: new focal chest signs on examination and at least one systemic feature (either a symptom complex of sweating, fevers, shivers, aches and pains and/or temperature of 380C or more). The most common causative pathogens of CAP include bacterial pathogens (for example Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae) and viral pathogens (for example RSV, influenza, COVID-19). If pneumonia is suspected, the patient should be referred for urgent medical attention, and prompt antibiotic treatment is recommended. The recommended duration of treatment if antibiotic prescribed is five days.
Community pharmacists can play a role in management of patients with CAP by checking antimicrobials are prescribed as per guidelines on antibioticprescribing.ie. It can be helpful to explain to people with CAP how long to expect to get better by. After starting treatment their symptoms should steadily improve, although the rate of improvement will vary with the severity of the pneumonia. Most people can expect that by one week fever should have resolved; by four weeks chest pain and sputum production should have substantially reduced; by six weeks cough and breathlessness should have substantially reduced; by three months most symptoms should have resolved but fatigue may still be present; and by six months most people will feel back to normal.
Advise people with CAP to consult their doctor if they feel that their condition is deteriorating or not improving as expected. Pharmacists can advise on treatment of pleuritic pain using simple analgesia and the importance of hydration. It could also be a good opportunity to discuss smoking cessation if appropriate and signpost to quit.ie.
Vaccinations (influenza, COVID-19 and pneumococcal vaccination) are key measures to reduce the burden of RTI and therefore reduce antibiotic use. Community pharmacists play a key part in the country’ vaccination programmes.
The following measures to contain respiratory secretions are recommended for all individuals with signs and symptoms of a respiratory infection and parents should educate children on respiratory etiquette:
Any infection, including RTIs could lead to sepsis. Advise the patient to seek medical attention if symptoms worsen rapidly or significantly, or they become systemically very unwell. Community pharmacists are very well positioned to be able to discuss sepsis red flags with patients and their carers. Refer to the HSE Sepsis page for further information and resources on sepsis (www2.healthservice.hse.ie/organisation/sepsis).
Table 5: Signs of sepsis
Signs and symptoms of sepsis in adults are:
Skin mottled and discoloured, new rash that is still visible when pressed on with a clear glass (glass test).
The signs and symptoms of sepsis in children are:
In children under three months: a fever of 38oC or more should prompt an urgent medical review.
Table 6: Commonly prescribed antibiotics in the treatment of RTIs
| Antibiotic | ‘Green’/’Red’ | Commentary |
| Phenoxymethylpenicillin | Green | Preferred agents if an antibiotic is deemed necessary for pharyngitis/sore throat/tonsillitis. Practice points: Recommend to take 30 minutes before a meal or two hours after food. |
| Amoxicillin | Green | Preferred option for acute sinusitis, community acquired pneumonia and infective exacerbation of COPD and is a second-choice option for pharyngitis/sore throat/tonsillitis. |
| Doxycycline | Green | Preferred first line agent in penicillin allergy for acute sinusitis, community acquired pneumonia and infective exacerbation of COPD. Practice points: ►Take with a glass of water and sit upright for 30 minutes; ► If gastritis is an issue, give with food or milk; ► Risk of photosensitivity: Advise use of sunscreen/sunblock; ► Separate administration of doxycycline from antacids, iron/calcium/magnesium/zinc-containing products by at least three hours or treatment failure may occur; and ► DO NOT OPEN CAPSULES. For swallowing difficulties, doxycycline dispersible tablets are available (unlicensed) and may be approved for reimbursement under the hardship scheme. |
| Cefalexin | Green | Cefalexin is the narrowest spectrum oral cephalosporin available. It is a second-choice option in pharyngitis/sore throat/tonsillitis. |
| Clarithromycin | Red | Less-preferred antibiotic, second-line option in penicillin allergy for pharyngitis/sore throat/tonsillitis, acute sinusitis, infective exacerbation of COPD and community acquired pneumonia. Practice points: ►Several significant drug interactions; and ► Avoid in patients with history of QT prolongation or arrhythmia. |
| Co-amoxiclav | Red | Co-amoxiclav is a very broad-spectrum agent and is a less-preferred antibiotic for most RTIs. It should be reserved for severe/worsening acute sinusitis and infective exacerbation of COPD as a second line option or when there is high risk of treatment failure. See antibioticprescribing.ie for advice on liquid preparations and higher dose recommendations. |