Home » OECD publishes report on key health indicators

The OECD, the Organisation for Economic Co-operation and Development, is an international organisation whose mission statement is “to build better policies for better lives”.
Health at a Glance is published by the OECD every two years and provides the latest comparable data and trends on different aspects of the performance of health systems in OECD countries. Its 2023 report was published in early November, and we provide details of some key indicators that will be of interest to pharmacists below.
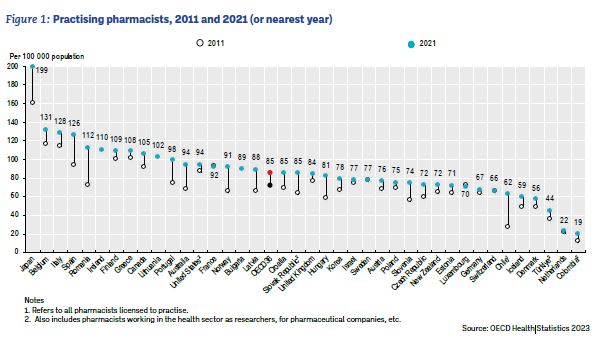
Between 2011 and 2021, the number of practising pharmacists per capita increased in OECD countries by 20% on average, to 85 pharmacists per 100,000 inhabitants, with Ireland at 110. This data from Ireland, reflects the data contained within the PSI register. The density of pharmacists varied widely across OECD countries, ranging from a low of 19 per 100,000 in Colombia to 199 per 100,000 in Japan.
Insert table at StatLink https://stat.link/me3jzc
Where pharmacists work also varied. In Canada, for example, in 2021 more than 75% of practising pharmacists worked in community pharmacies, while 20% worked in hospitals and other healthcare facilities. In Japan, around 59% of pharmacists worked in community pharmacies in 2020 while around 19% worked in hospitals or clinics, and the remaining 22% in other settings.
Insert table available at StatLink https://stat.link/2vkuc7
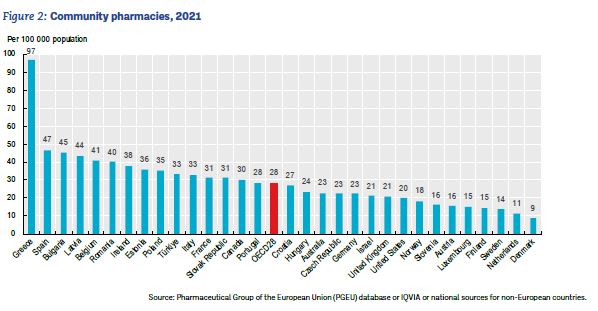
In 2021, the number of community pharmacies per 100,000 people ranged from 9 in Denmark to 97 in Greece, with an average of 28 across OECD countries with comparable data. In Ireland the figure was 38. For most countries there has not been much change over time, although one exception is Denmark, where the community pharmacy density almost doubled between 2011 and 2021. The variation in community pharmacy density across countries can be explained in part by differences in common distribution channels. For example, some countries rely more on hospital pharmacies to dispense medicines to outpatients. Denmark has fewer community pharmacies, but these are often large, and include branch pharmacies and subsidiary pharmacy units attached to a principal pharmacy. In Australia, with an average of around 23 community pharmacies per 100,000 people, the minimum distance between pharmacies is regulated.

“ Between 2011 and 2021, the number of practising pharmacists per capita increased in OECD countries by 20% on average, to 85 pharmacists per 100,000 inhabitants, with Ireland at 110.”
The report cites that, “Pharmaceutical consumption has been increasing for decades, driven by a growing need for medicines to treat age-related and chronic diseases, and by changes in clinical practice”. A section in the report examines the consumption of four categories of medicines used in selected chronic conditions: antihypertensives, lipid-modifying agents (such as cholesterol-lowering medicines), antidiabetic agents and antidepressants.
Consumption of antihypertensive medicines in OECD countries increased by around 8% on average between 2011 and 2021, but nearly tripled in Chile. It remained highest in Germany, which reported consumption levels almost five times those seen in Korea.
Much greater growth was seen in the use of lipid-modifying agents, with consumption in OECD countries increasing by almost 60% between 2011 and 2021 on average. Denmark, the United Kingdom and Norway reported the highest levels of consumption per capita in 2021, with over a five-fold variation in consumption levels across OECD countries.
The use of antidiabetic medications also grew dramatically, by 30% over the same period, and more than doubled in Canada and Chile.
Consumption of antidepressant medicines increased by nearly 50% in OECD countries between 2011 and 2021, more than tripling in Chile and doubling in Korea, Latvia and Estonia. There was significant variation between countries in 2021, and Iceland reported the highest level of consumption, at a rate eight times that of Latvia.
More recently, pharmaceutical consumption in each of these four categories increased by around 10% in OECD countries on average between 2019 and 2021, except for antihypertensive medicines, where consumption remained relatively stable, and even decreased in some countries.
The Report states that, “All OECD countries view generic and biosimilar markets as an opportunity to increase efficiency in pharmaceutical spending, but many do not fully exploit their potential”. In 2021, generics accounted for more than three-quarters of the volume of pharmaceuticals sold in Chile, Germany, New Zealand, the United Kingdom, the Netherlands, Canada and Latvia, but less than one-quarter in Switzerland and Luxembourg. In Ireland the figure was 44%.
“Differences in market structures (notably the number of off-patent medicines) and prescribing practices explain some cross-country differences, but generic uptake also depends on policies. In Austria, for example, generic substitution by pharmacists is not permitted, while in Luxembourg, generic substitution by pharmacists is limited to selected medicines.
The Report also describes incentives that have been introduced in some countries for physicians, pharmacists and patients to boost generic markets; “Over the last decade, France and Hungary, for example, have introduced incentives for general practitioners to prescribe generics through pay-for-performance schemes. In Switzerland, pharmacists receive a fee for generic substitution; in France, pharmacies receive bonuses if their substitution rates are high. In many countries, third-party payers fund a fixed reimbursement amount for a given medicine, allowing the patient a choice of the originator or a generic, but with responsibility for any difference in price.”
The report states that, “the market entry of biosimilars creates price competition, thereby improving affordability. However, the extent of biosimilar penetration in a country will depend on the reimbursement status of the biosimilar medicines.” It provides the example of Ireland, where only one of the five biosimilars licenced by the European Medicines Agency for epoetin alfa is available on the reimbursement list.
On average across OECD countries, 43% of people in the lowest income quintile report a longstanding illness or health problem compared to 27% of people in the highest income quintile. Ireland is among the countries with the largest income gap. Along with Lithuania, Belgium and Estonia, people in the lowest income quintile in Ireland are two or more times as likely to have at least one longstanding illness or health problem compared to people in the highest income quintile. The income gap is smallest in Italy and Turkey, where individuals in the lowest income quintile are slightly less likely to report living with a longstanding illness or health problem compared to individuals in the highest income quintile.
Over the last decade, daily smoking rates decreased in 31 of the 35 OECD countries. On average, they fell from 20.6% in 2011 to 15.9% in 2021, and Ireland is one of the countries with the largest reduction rates. Alongside Norway and Estonia, Ireland had a reduction above 8 percentage points.
While more than one in two adults reported consuming at least one vegetable per day, only one in seven reported consuming the five or more portions of fruit and vegetables per day recommended by WHO. In 2019, 15% of adults reported eating five or more portions of fruit and vegetables per day on average across 30 OECD countries. Ireland was among the countries with the highest proportions of adults reporting consuming five or more portions of fruit and vegetables per day, along with the United Kingdom, Korea, Israel and the Netherlands (30% or above). Women are more likely than men to consume five or more portions of fruit and vegetables per day in all OECD countries except Greece and Korea. Ireland was among the countries with the widest gender gap, along with Denmark and Finland.
Across OECD countries, 56% of pharmaceutical costs were financed by government or compulsory insurance schemes. Ireland was among the countries with the most generous coverage (82%), along with France (83%) and Germany (82%).
In the EU, the 2021-22 influenza season signalled a return to increased influenza virus activity after the low-level circulation during the COVID-19 pandemic. The WHO recommends that 75% of people aged 65 and over should be vaccinated against seasonal influenza. This target was only attained in the United Kingdom (81%), Korea (80%) and Denmark and Ireland (75%) in 2021, whereas the influenza immunisation rate among this vulnerable group was very low at below 15% in Latvia, Poland and the Slovak Republic.
Health at a Glance is available at oecd.org > Topics > Health > Health at a Glance.
Siobhán Kane

Editorial Manager, IPU
Highlighted Articles