Home » Northern Ireland’s Pharmacy First Service — how it works in practice

Following the publication of the report of the Expert Taskforce to Support the Expansion of the Role of Pharmacy in August 2024, the Minister for Health established a Community Pharmacy Expansion Implementation Oversight Group (IOG), who have been tasked with implementing the recommendation that pharmacists should be able to prescribe for a range of common conditions. The work of this group is ongoing, with an aim to have all the key enablers in place by the end of 2025 to support the implementation of a national Common Conditions Service.
Pharmacies in Northern Ireland are well placed within communities and are essentially an ‘open door’ to the health service, offering free independent health advice without the need for an appointment. The Northern Ireland Pharmacy First Service, launched in 2019, is a service whereby patients are encouraged to consult with their community pharmacist first rather than their GP, for a list of common conditions. The aim of a Pharmacy First Service is to move activity, including consultations and advice for common conditions, from GP practices to community pharmacies.
There are three ways in which a patient can participate in the service:
When a patient/parent/guardian presents at the pharmacy with symptoms that fall into one of the therapeutic areas covered by the service, the pharmacist carries out a consultation/assessment in the consultation area, or other private area of the pharmacy. Outcomes of the consultation include the provision of advice only, advice plus treatment from the service formulary (up to a maximum of two products per patient as appropriate) and/or referral to the GP or other healthcare services, as appropriate.
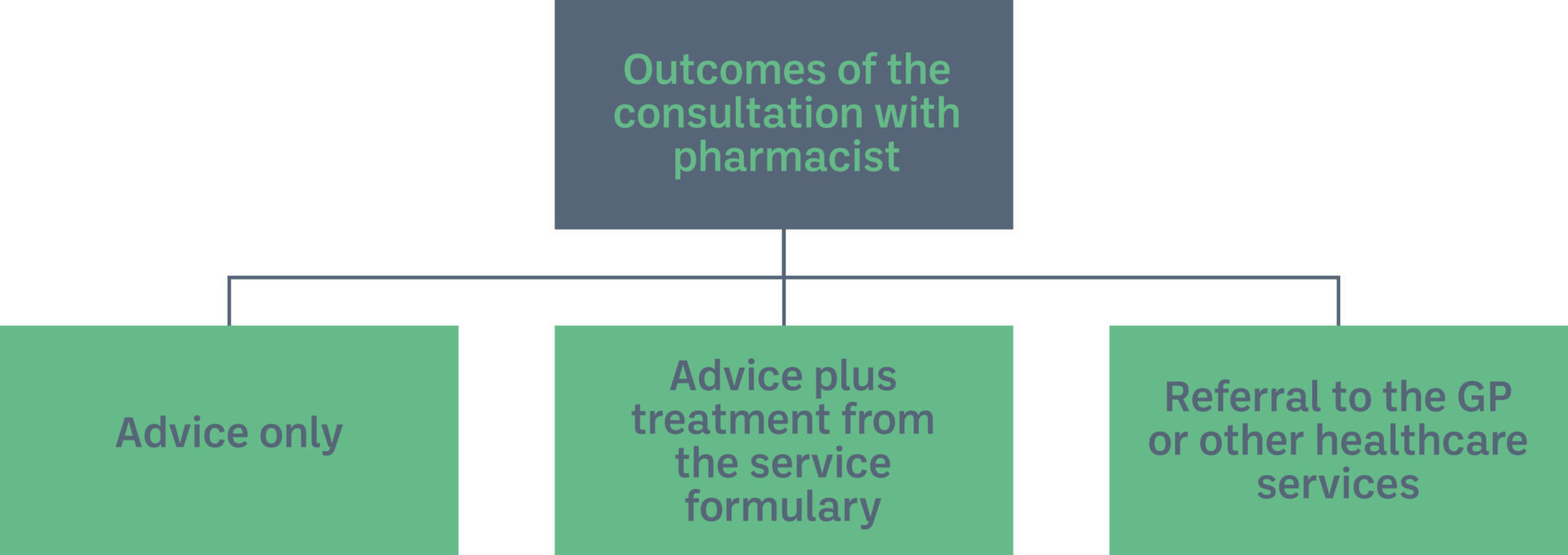
Figure 1: Outcomes of consultation under Pharmacy First Service
Services provided
The service includes three core services:
Pharmacy First for Sore Throats was introduced in November 2024 to support the health service in managing winter pressures and it has been extended until the end of August 2025. It is hoped this will become a permanent service within Pharmacy First. A Shingles pilot also commenced in early 2025 with a view to assessing the feasibility of ongoing delivery in practice and hopefully incorporate the condition into the Pharmacy First Service on a permanent basis too.
In 2023, over 150,000 people used the Pharmacy First Service for one of the 13 everyday health conditions. In 2024/2025, over 40,000 Pharmacy First consultations were undertaken for UTIs and EHC. In May 2024, the Department of Health unveiled plans for pharmacies to treat six new conditions, offer two new services and run various pilots in its community pharmacy strategic plan. The new services are set to be introduced in the period up to 2030 — “subject to securing the necessary funding”.
Patients avail of the service free at the point of delivery and pharmacists are reimbursed for provision of a consultation and, where appropriate, for the supply of a medication. The consultation fee varies for different services with consultations for everyday health conditions paid under a tiered model and a fee per consultation of £32/£30/£25 paid for consultations conducted under the Pharmacy First Sore Throat/UTI/EHC and Shingles services. This fee includes the cost of consumables where appropriate. A consultation fee can be claimed provided the consultation relates to a condition detailed within the service and the relevant paperwork has been completed at the time of the consultation. Medication supply is reimbursed separately.
A number of evaluations of the Service have been conducted. An evaluation of 1,032 pharmacist consultations for uncomplicated UTI in women aged 16 to 64 years provided between July and November 2021 showed that 82 per cent of patients received antibiotic treatment for their UTI and 8 per cent of patients required onward referral to another healthcare professional. Patients reported that the advice they received was helpful (98 per cent), they would recommend the service to family and friends (99 per cent) and that if the service had not been available, they would have contacted their GP (79 per cent) or out of hours medical services (21 per cent). 81 per cent of GP practices agreed that the service should be considered for rollout to all community pharmacies.
An evaluation of the Pharmacy First for Sore Throat Service for patients aged five years and over published in June 2024, showed that an antibiotic was only supplied in 25 per cent of cases with patients who did not need antibiotics managed with advice on self-care and, where necessary, analgesia, such as paracetamol or ibuprofen. This Service utilises both point of care testing and a clinical scoring system to support diagnostic confidence of suspected group A streptococcus infection. 96 per cent of patients indicated that they would be likely or very likely to use the service again and to recommend it to family and friends; 93 per cent indicated they received advice on how to manage symptoms from the pharmacist and that this advice was helpful; and 81 per cent felt confident to manage symptoms themselves in the future.
Provision of the Pharmacy First Service through community pharmacies:
More information on the Pharmacy First Service is available at communitypharmacyni.co.uk > Services > Pharmacy First.
Katherine Kidd

Head of Pharmacy Development, Community Pharmacy Northern Ireland
Highlighted Articles