Home » National ePrescribing Project
Electronic Prescribing (ePrescribing) has been implemented in many healthcare systems internationally. It is one of the digital technologies that has the potential to transform healthcare by improving the efficiency and coordination of care, supporting people to manage their own medications and changing the way people engage with services and professionals. In this article, Bríd Ryan, Clinical Lead for ePharmacy in the HSE, provides an overview of ongoing and upcoming initiatives around ePrescribing.

ePrescribing is part of the modern eHealth infrastructure identified as a key strategic goal of the Sláintecare programme. There is a drive and an urgency to implement ePrescribing in Ireland, and the National ePrescribing Project has been established to plan, action and deliver ePrescribing.
Electronic prescribing can mean different things to different people. The secure email of prescriptions, for example Healthmail, is a type of ePrescribing, so too is closed loop prescribing, dispensing and administration of medicines. There have been advantages from the implementation of the secure email of prescriptions using Healthmail; however, this is a one-way communication of uncoded information. Pharmacy staff must still type in patient and medication details into the pharmacy dispensing systems; therefore, the risk of transcription and selection errors remains.
There are significant benefits to gain by progressing to ePrescribing where semantic interoperability is achieved and there is seamless, digital flow of coded structured patient medicines information across healthcare settings (Figure 2). The Healthcare Information and Management Systems Society (HIMMS) explains that, “semantic interoperability takes advantage of both the structuring of the data exchange and the codification of the data including vocabulary so that receiving information technology systems can interpret the data”.

Delivering the vision for ePrescribing (Figure 1), across all care settings will be a multi-phase project. The aims of the National ePrescribing Project in the first phase are to:
Connecting systems might sound straightforward; however, realising the true benefits of digitisation means that we will need to agree on standards and adopt them. These standards will provide a common language and a common set of expectations that enable this semantic interoperability between systems and/or devices. Examples of standards are:
This standardisation will ensure that prescribing and dispensing information, shared between different systems, will be accurately interpreted by the receiving system. All of this has to be underpinned by appropriate approaches to medicines safety.
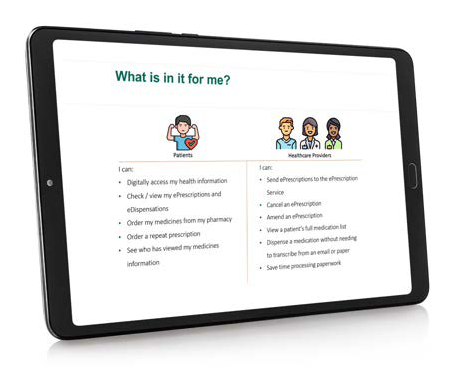
In early 2023, the project team carried out an early stakeholder engagement with patients, prescribers and pharmacists. The aim of this was to meet and consult with key stakeholder groups who will use ePrescribing on a regular basis to receive or deliver healthcare. We wanted to understand how the high-level plans presented (Figure 2) would fit with their needs now and in the future. The aim was also to identify potential gaps in the high-level plans and inform current and future project plans. The stakeholder engagement explored the benefits of ePrescribing for the stakeholder groups and any potential barriers to ePrescribing that participants wished to share.
The engagement was carried out in two stages. In the first stage, qualitative feedback was gathered with a series of semi-structured face-to-face meetings. We met patients, pharmacists and prescribers separately. Eight meetings of 90 minutes duration took place and explored the opinions and experiences of each group. In the second stage, this qualitative feedback was collated and presented to all participants in the form of an online questionnaire. The questionnaire then prompted participants to consider and prioritise a number of statements in order to gather quantitative feedback from the group as a whole.
Forty-four people participated in the first round of face-to-face meetings. The participants actively engaged and provided extensive information on what mattered to them. There were forthright conversations, and participants posed questions for the project team to reflect on. Twenty-seven responses were received to the online questionnaire in the second round. The following three sections summarise the results of the engagement process. The full report is available to download on the eHealth ePrescribing webpage.
The focus during the patient meetings was on how ePrescribing could positively contribute to medication safety, and how it would empower patients and result in more efficient interactions with healthcare services for patients. This was matched by the online questionnaire, which ranked the most important benefits of ePrescribing in that order.
Prescribers felt that access to accurate and secure medication information would be invaluable and enable them to make more informed decisions when delivering care. This was summed up by one participant who said, “it would be nice to have a universal system that everybody would know how to use, and medications won’t get missed or polypharmacy could be addressed”. Pharmacists highlighted how patients transitioning between healthcare settings would benefit as pharmacists and medical teams would have access to a greater level of knowledge of all prescribed and dispensed patient medications — “that more complete record would just be a bit of a game changer really”.
The positive effect on patient efficiencies was noted. Patients believed ePrescribing would make their interactions with prescribers and their community pharmacy easier. The addition of a patient application (app) would allow patients to have greater accessibility to information on their prescribed and dispensed medications. It was felt that this could be useful in promoting improved medication management and compliance by patients.
Participants were asked about features they would like to see in the short and long-term from ePrescribing. After the medication list, the second most important ePrescribing feature was the ability to document and view the indication for each medication. In a similar vein, documenting reasons for stopping medications was a significant feature that would reduce unnecessary calls and enable safer care during transitions of care. Other features discussed were user-friendly systems, streamlining of reimbursement processes, additional clinical decision support functions and real time tracking of prescriptions, so patients would be informed when items are prepared and ready for collection. A desired feature requested by patients that was not originally included in the high-level outline, was the ability for patients to contribute to their medication list and document additional medications and/or supplements, that they are taking. The need for a robust privacy approach to safeguarding patients’ data was also discussed.
Participants understood the scale of the change ahead for patients, prescribers and pharmacy teams and flagged this as the key barrier to ePrescribing. Other barriers discussed were trust in the security of ePrescriptions, technological literacy, scale of information, education and training required and fear of system breakdown. Patients posed numerous questions in relation to privacy and spoke about their concerns about sensitive patient information being shared across electronic platforms and accessed by multiple healthcare professionals.
The early stakeholder engagement process has shown the interest, enthusiasm and desire for ePrescribing. The process has shown that the high-level plans will meet many expectations. It also outlined additional areas to consider the feasibility of now, or in the future. There was an awareness and appreciation that this is a complex piece of work which will develop with time. The need to be honest in what we will achieve and deliver at each stage was heard.
In tandem with the early stakeholder engagement, the project team carried out a market consultation exercise. This is a structured dialogue with potential vendors before we run a formal public procurement for an ePrescription Service provider. The purpose of this was to:
The market consultation was advertised on eTenders. Ten responses were received and the ePrescribing Project Team met with nine of the vendors. From these meetings, we know that the technical functionality required for a National ePrescription Service is available to purchase from the market. The real benefit of this exercise was to meet vendors with experience in ePrescribing. The take-home message from them was the importance of standardisation as this will lead to good quality data. Without good data quality, the vision of a seamless, digital flow of patient’s medicines information across healthcare settings will be a challenge.
ePrescribing is a complex but achievable body of work

Theodore Roosevelt is quoted as saying, “Nothing in the world is worth having or worth doing unless it means effort, pain, difficulty”. To date, a lot of effort has been put into this project by patients, pharmacists and prescribers. The willingness to critically review documents, meet either during or out of work hours, and collaborate with the project team is greatly appreciated. ePrescribing is a complex but achievable body of work. We have yet to hit the pain and difficultly, but the vison of seamless, digital flow of patient’s medicines information across healthcare settings will make that worthwhile.
If you are interested in this topic, we recently presented at an IIOP webinar giving an overview of the project, and this can be watched through the IIOP website. Further publications and updates will be accessible on the eHealth Ireland ePrescribing webpage.
References available on request.
Bríd Ryan

Clinical Lead ePharmacy, HSE
Highlighted Articles