Home » Managing mild to moderate acute pain
This article from pharmacist Amy Oates focuses on mild to moderate acute pain, including aims of pain management and current guidance that is available. Ms Oates will also discuss common over-the-counter medications that are available to treat this type of pain and when it is appropriate to recommend them.

Pain is defined by the International Association for the Study of Pain as “an unpleasant sensory and emotional experience, associated with actual or potential tissue damage, or described in terms of such damage”. Pain is always a personal experience and a person’s report of their pain should be respected.
Pain can be divided into two categories: acute and chronic. Acute pain lasts for less than three months and acts as a warning to alert the body to a problem. The majority of acute pain episodes arise mainly from musculoskeletal conditions. Examples of acute pain can include sprains and strains, headaches and toothache. Chronic pain, on the other hand, persists beyond the expected time of healing or beyond three months. Chronic pain may be attributable to an event, such as an accident, a condition (for example, arthritis) or a non-traceable occurrence. It is classified as a disease, degrading health and functional capability.
When a patient seeks pain relief for acute pain which is mild to moderate it is important to determine the desired outcomes for the patient. The characteristics patients often look for include good pain relief, fast onset of action and long duration of action.
The National Institute for Health and Care Excellence (NICE) has produced a Clinical Knowledge Summary (CKS) for mild-to-moderate pain. This CKS provides practitioners with a summary of the current evidence base and practical guidance. It recommends that the underlying cause of the pain should be treated whenever possible and that a full therapeutic dose of drug is used before switching to a different analgesic.
NHS England provides guidance on a range of conditions that can be treated with over-the-counter medicines. Patients are firstly encouraged to self-care for acute pain conditions such as aches and pains, headache, period pain, self-limiting musculoskeletal pain, sprains and strains and toothache. Self-care however presents patients with a broad range of oral OTC analgesics, alone or in combination with other ingredients, which makes appropriate medicine selection confusing. Pharmacists and their teams can ensure the best treatment for patients based on their needs through appropriate consultations and recommendations based on clinical guidelines.
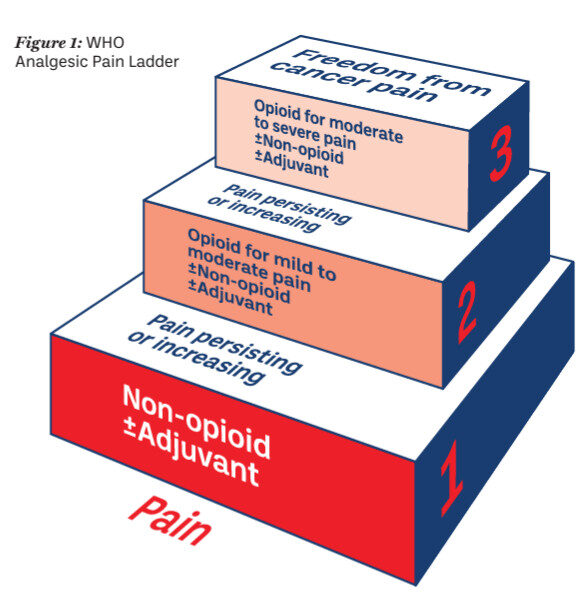
The World Health Organization (WHO) analgesic ladder was introduced in 1986 as a tool for the treatment of pain caused by cancer (see Image 1). This step-wise approach to analgesia can be applied to the management of acute pain.
The ‘Pain Ladder’ recommends that patients always begin with the lowest form of appropriate pain-relief for the shortest amount of time for their symptoms. This will reduce the incidence of side effects and the risk of dependence.
Over-the-counter analgesics can be used according to this tool, using a stepwiseapproach.
Step 1 involves starting with simple analgesics i.e. paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs)
Step 2 introduces weak opioids i.e. tramadol and codeine
Step 3 involves the use of strong opioids .e. morphine, fentanyl, oxycodone, pethidine
The WHO analgesic ladder provides a very useful guideline for pain management and can be used by pharmacy teams to aid treatment recommendations. At every step of the analgesic ladder non-opioid analgesics form the basis of pain management and it is advised to use an analgesic to the maximum therapeutic dose before adding in another agent. For the management of acute pain we will focus on simple analgesia and weak opioids in this article.
Image 1: WHO Analgesic Pain Ladder
First-line treatment recommendations vary depending on the type of pain and additional factors, including clinical presentation, patient comorbidities and contraindications. All of these factors need to be taken into account. The NICE CKS recommends that combination analgesics should be avoided as first-line treatment, as single constituent analgesics allow independent titration of each medicine. Pharmacists should always consult the summary of product characteristics and advise the patient on correct dosage, side effects and to read the patient information leaflet.
Paracetamol is a suitable first-line choice for most adults with mild-to-moderate pain. It is specifically recommended first-line for management of strains and sprains. It does not however have anti-inflammatory properties. Paracetamol has no known GI, renal or cardiac adverse effects at usual over-the-counter doses. However, pharmacists and their teams should always check with the patient when paracetamol was most recently taken how much was over the previous 24 hours to prevent overdose. It is important to ask about other prescribed medication, as some patients might not be aware if they contain paracetamol.
“Pharmacists and their teams can ensure the best treatment for patients based on their needs through appropriate consultations and recommendations based on clinical guidelines.”
Paracetamol started at low dose, can be increased to a maximum of 1,000mg four times per day before switching to or combining with another analgesic.
Ibuprofen is the first-line recommendation for a wide range of pain, including lower back pain, period pain and toothache.
NSAIDs or aspirin should not be sold to patients with active gastrointestinal bleeding or active GI ulceration, history of GI bleeding related to previous NSAID therapy or history of recurrent GI ulceration. They are also contraindicated in patients with a history of hypersensitivity to an NSAID, or allergic reactions from use resulting in asthma, rhinitis, angioedema or urticaria; severe heart failure, liver impairment or severe kidney impairment. Caution is also required in older people; people with comorbidities; people who take medicines that may interact with a NSAID; and those at increased risk of GI or cardiovascular adverse effects.
Ibuprofen recommended at a low dose of 200mg – 400mg three times per day to start can be increased to 1,200mg daily, if a higher dose is required and not contraindicated.
Codeine is often combined with paracetamol, or ibuprofen in OTC preparations and can be offered for a variety of acute aches and pains. It is not recommended as a first-line treatment. Codeine containing products combined with paracetamol should only be offered for managing acute lower back pain if an NSAID is contraindicated, not tolerated or has been ineffective. As per NICE guidance, opioids should not be recommended for the acute treatment of tension-type headaches or migraines.
PSI Guidance states that codeine containing medicines should only be supplied when necessary, under a pharmacist’s supervision, and not available for self-selection by the public (see Non-Prescription Medicinal Products Containing Codeine: Guidance for Pharmacists on Safe Supply to Patients, available at psi.ie > Practice Supports > Guidance and Guidelines for Pharmacists and Pharmacies). Codeine products should only be considered when other analgesics such as paracetamol, aspirin or ibuprofen has not been effective. If codeine is deemed appropriate to recommend, it is important that patients are advised to use for the shortest time possible and for no longer than three days. Pharmacists and their teams must take the time to counsel patients effectively on how to use codeine products, and the risks associated with prolonged use. Long-term use of weak opioids such as codeine can result in tolerance and dependence.
Genetic differences in the expression of the CYP2D6 enzyme results in differences in the extent to which codeine is metabolised. Patients who metabolise codeine very rapidly (ultra-rapid metabolisers) are at increased risk of developing adverse effects of opioid toxicity, even at low doses, hence codeine containing medicines are contraindicated in known ultra-rapid codeine metabolisers.
Patients should also be counselled in the course of each supply in respect of other potential adverse reactions or side effects, including nausea, constipation, dizziness and drowsiness (which may impair their ability to drive safely). They should also be counselled, as appropriate, regarding the contraindications for use, drug interactions, or existing medical conditions, which may preclude the use of these medicines. The need for safe storage of these medicines should also be addressed with patients.
Table 1: Common acute pain conditions and the recommended, over-the-counter, evidence-based analgesia
| Lower back pain | NSAID (for example, ibuprofen 400mg three times per day) at the lowest possible dose for the shortest possible time. Do not offer paracetamol alone. |
| Period pain | NSAID (for example, ibuprofen 400mg three times per day) unless contraindicated. Paracetamol can be used if a NSAID is contraindicated or provides insufficient pain relief. |
| Sprains and strains | Paracetamol (for example, paracetamol 500mg to 1g four times per day) or topical NSAID (for example, ibuprofen or diclofenac gels) are recommended first-line. Consider oral NSAID (for example, ibuprofen 400mg three times per day) 48 hours after the initial injury if needed. |
| Tension type headache | Aspirin (for example, aspirin 300mg three times per day), paracetamol or NSAID, taking into account patient preference and comorbidities. |
Sources: National Institute of Health and Care Excellence
Pharmacy is often the first point of contact for patients experiencing pain. There are a wide range of guidelines available to help pharmacists and their teams offer the best treatment recommendations for their patients. When a patient presents looking for pain relief we first need to understand what type of pain the patient is experiencing and the outcomes they are seeking. The underlying cause of the pain should be treated when possible. It is important to involve patients in their treatment through an effective consultation. Pharmacists and their teams should first determine what analgesics the patient has taken previously, if any, and find out if they have been taking them appropriately. We need to ensure we provide patients with information and advice to support the use of pain relief. The HSE A to Z of conditions, available at www2.hse.ie/conditions, is a great source of up to date information and advice on management of different types of pain.
References available on request.
Amy Oates MPSI

Highlighted Articles