Home » Management of Codeine dependence

Codeine phosphate is a mild to moderate opioid (narcotic) analgesic and has weak cough suppressant activity. Codeine, due to its potential for misuse, is a controlled drug under the Misuse of Drugs Acts 1977 and 1984. Low dose preparations are regulated as a Schedule 5 controlled drug which must be sold under the direct supervision of a pharmacist and must be sold with specific counselling. Specifics of the conditions of sale are described in the Pharmaceutical Society of Ireland’s (PSI) Non-Prescription Medicinal Products Containing Codeine: Guidance for Pharmacists on Safe Supply to Patients.
Codeine acts by stimulating opioid receptors in the body. This may be of benefit in mild-moderate acute pain for short-term relief. Recommended dosing schedules are as follows:
It is sold over the counter (OTC) in combination with other painkillers, mainly as:
Stimulation of opioid receptors brings some other effects such as constipation, dizziness, drowsiness, irregular heartbeat (arrhythmias), dry mouth, elevated mood, flushing, hallucinations, nausea/vomiting (particularly when starting), urinary retention (unable to pass urine) and vertigo.
The use of opioids whether prescribed or non-prescribed comes with a risk of effects on the Central Nervous System such as sedation/drowsiness, respiratory depression (difficulty in breathing) and opioid overdose. Use should be limited to the lowest dose possible for the shortest duration.
The use of codeine appears to differ with age, see graph below, with some evidence of a greater level of use in young women and those over 65 years, which may indicate a cohort seeking relief from non-managed pain, for example poorly controlled menstrual pain or osteoarthritis.
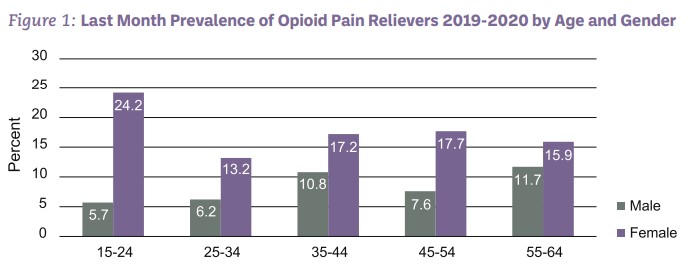
Source: The 2019-20 National Drug and Alcohol Survey, HRB
There is also a risk of dependency with prolonged use, for example three months or longer. Patients should be made aware that ongoing use can lead to dependence and addiction, as some people become dependent as a result of increasing use of codeine-containing products to self-manage pain due to menstrual disturbances or following an acute event such as a car accident. Those with a current or previous history of substance misuse or mental health disorders are at an increased risk of developing dependency.
Codeine may be used in combination with other products, which reduce respiration or depress the Central Nervous System such as benzodiazepines, alcohol or other opioids. This increases the potential for a drug overdose, which can be fatal. Codeine was found to be present in 167 deaths in 2008-2017 (the last year of National Drug Related Death Index statistics), see the graph below. In 87% of these deaths other substances were found in the body.
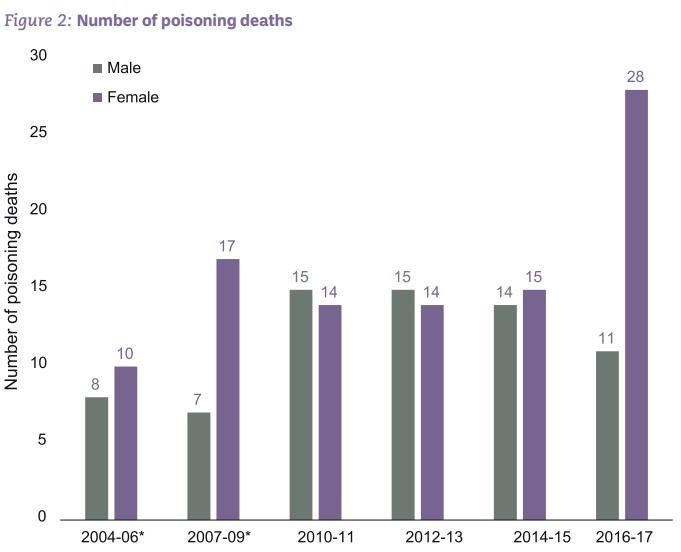
Year of death (*3 years combined to account for small numbers)
(Health Research Board, 2018)
Many people presenting for treatment are solely codeine dependent and report that they would never consider using illegal opioids such as heroin. There are some people who use codeine along with other substances, i.e. polysubstance misuse.
Attempts to cut down should be done slowly to reduce the risk of withdrawal symptoms and this may take many weeks or months. Withdrawal symptoms can be very unpleasant and may include, severe stomach cramps, diarrhoea, headache, restlessness, irritation, anxiety, insomnia, and heightened pain sensitivity. Many people who become aware they have become dependent on codeine find that they cannot stop due to the withdrawal symptoms. Withdrawal symptoms upon stopping may persist for up to ten days at a level which is severe enough to interfere with daily duties such as working, or daily activities and relationships.
Reflection
Consider the following two scenarios whereby two different customers ask for a codeine containing product for different reasons. Consider the scenarios from the perspective of the medicines counter assistant and the customer requesting the product.
Scenario:
A woman in her mid-20s asks for a codeine/ibuprofen containing product or menstrual cramps. She was also in last month requesting the same thing again.
| Customer One | |
| OTC Assistant thoughts | Customer thoughts |
| I’m sure I recognise her from last week asking for the same thing? I wonder if her pain is being well managed? | I must get something from my GP for these cramps but I can’t get an appointment. |
| I need to ask her the same set of questions as last week. | Why do they have to ask all these questions, I’m not doing anything wrong! |
| Possible suggestions | |
| Effective use of questions helps to determine whether pain is being managed effectively Suggest a trip to the GP if this is not strong enough or if analgesia is needed for more than three days at a time. The GP may be able to prescribe non-opioid based analgesia and prescribe enough to do for a few months. | I really should book that GP appointment or see a Family Planning clinic. I use the entire packet every month and I still have pain. |
| Customer Two | |
| OTC Assistant thoughts | Customer thoughts |
| I’m sure I recognise her face from last week asking for the same thing? I wonder if her pain is being well managed? | I need a few packets to help me cope with things, I have to work later, and I won’t be able to if I have a splitting headache and tummy cramps. |
| I need to ask her the same set of questions as last week. | I hope I answer all the questions correctly. |
| Possible suggestions | |
| Suggest a trip to the GP if this is not strong enough or if analgesia is needed for more than three days at a time. An experienced staff member may feel confident enough to highlight the potential for dependency and open up the option for treatment. If in doubt that the criteria for sale/supply are not met, there is always the option of declining the sale in an empathetic manner. | I never thought about the fact I might be dependent on these tablets! I would love to be able to stop taking them . . . maybe I should ask for help? |
This may differ depending upon personal circumstances and the degree of dependency. Factors to consider are:
Be aware that many people may take a defensive position when asked about dependency and that adopting an empathetic tone of voice and respecting customer privacy may help.
Continued use may result in physical damage to the body often related to the non-codeine element of the codeine-containing product such as stomach ulceration, bleeding from the bowel, kidney failure, urinary function problems, chronic constipation and iron-deficient anaemia (possibly due to malabsorption and gastro-intestinal bleeding). Some people may present to their GP or hospital departments with these symptoms without disclosing their chronic use of codeine-containing products, which poses a difficulty for doctors trying to identify the cause of the symptoms.
Hepatic failure or overdose is also a possibility due to excessive ingestion of products containing paracetamol and codeine.
In some cases, a physical, psychological, financial or social crisis may be a trigger for people to seek help. The emotional and financial strain of sourcing a sufficient supply of codeine to manage symptoms can be enormous and time-consuming. Addiction services reported an increase in self-referrals during the COVID lockdowns as access to community pharmacies was more restricted and public transport was reduced.
Some people may be able to cut down themselves, and some may need support from an addiction counsellor if available to them, particularly in the first few months. For some the realisation that there is a risk of dependency, or recognition that they are in some way dependent may be enough of a trigger to reduce or stop use. Some GPs may be able to offer support. A slow titration down may be required over many weeks to reduce the risk of unmanageable withdrawal symptoms.
Many people will need opioid substitution therapy, now called opioid agonist therapy (OAT), in the form of a longer acting opioid such as buprenorphine or methadone. OAT will reduce opioid craving and opioid withdrawal symptoms and remove the need to endlessly seek a supply of codeine. It will also remove ingestion of the second analgesic in codeine products such as paracetamol and ibuprofen, which can cause serious side-effects with longer term high dose use.
Buprenorphine is usually considered the first line for codeine dependency for a number of reasons. Firstly, there is less stigma associated with its use and it is a sublingual (under-the-tongue) tablet, which may be more preferable to liquid methadone. It doesn’t cause as much respiratory depression compared with methadone, which makes it safer in an overdose situation. Buprenorphine has both some agonist (stimulating) effects and also some antagonistic effects and overall, this means a lower level of opioid effects compared with methadone. For patients this means they may feel less drowsy and may feel clearer headed than if they were taking other opioids.
Currently any OAT needs to be started by an experienced General Practitioner or Consultant Psychiatrist specialising in addiction, usually based in an addiction clinic or in GP practice. The patient will be allocated to a specific pharmacy, preferably one that is convenient to the person’s home or place of work. Feedback from patients is that they report their symptoms and wellbeing improves greatly once they are started on OAT, and they can focus on building back their lives again. The physical side-effects of taking long term ibuprofen/codeine use such as low-iron/anaemia, kidney problems, lethargy, stomach upset, chronic constipation, etc, generally improve with supportive treatment. In some cases, however, the damage may be irreversible.
The HSE Drugs and Alcohol Confidential Helpline 1800 459 459 is a useful starting point when seeking help for codeine dependency. Trained staff will carry out a screening process in order to direct the caller to the most appropriate service. Alternatively, a list of local services is available under the Services section on www.drugs.ie (choose Opioid Substitution Treatment from the drop-down menu of Service type).
GPs can refer the person to an addiction clinic for assessment, or most clinics will have a self-referral system for assessment. The assessment will look at the level of support needed, whether this is addiction support/counselling or OAT. Addiction counselling focuses mainly on introducing techniques to cope with cravings and withdrawal symptoms. Counselling may not go into deeper issues such as dealing with trauma or abuse until the addiction element has stabilized, and then only if needed.

In order to ensure the safe use of codeine-containing products and to increase awareness that help is available for codeine dependency for those who want it, it is important to:
Practitioner health provides confidential, trusted support to healthcare professionals who may have mental health issues such as stress, anxiety or burnout or who may have a substance misuse problem. See practitionerhealth.ie, email confidential@practitionerhealth.ie, or call 01 278 9369.
References available on request.
Norma Harnedy

National Liaison Pharmacist, HSE Addiction Services
Highlighted Articles