Home » Keeping a medicines list

A medicines list is a list, compiled by a patient or their carer, that notes all medicinal products that a person is taking. In this article, Patients for Patient Safety Ireland, the IPU and the HSE have worked together to explain why such lists are important and how they can improve patient safety.

Unsafe medication practices and medication errors are a leading cause of avoidable harm in healthcare across the world. Transitions of care are high risk for medication errors. With traditional medication history taking, Irish research has shown that 41% of patients had at least one medication error at admission. At the time of discharge, 56% of patients experienced prescribing errors and miscommunication.
A medicines reconciliation process is needed at transitions of care to interview the person and verify with at least one reliable source of information (for example, by contacting the patient’s community pharmacy or GP). People who use a medicines list are more likely to be able to recall their medicines accurately at admission than those who do not.
A medicines list is a self-compiled list which include all medicinal products that a person takes. Prescription and over-the-counter medications, vitamins, supplements, and alternative medicines should all be included on the list. Details of the relevant doses for the medications, frequency of use and indication, should also be included.
The list is a tool that helps people taking medication to understand what medications they are taking and for what reason. Ideally it should be completed by the person taking the medication. Where this is not possible, family members and/or carers can also support with compiling the list. Compiling the list empowers patients to better know and understand their medicines.
The list is then used by the person to share with healthcare professionals at appointments, or whenever they are asked about their medications.
“A medicines list is a simple yet powerful step that can improve patient safety”, according to Bernie O’Reilly of Patients for Patient Safety Ireland. “Research from the WHO and the HSE confirms that empowered patients who know and understand their medications, dosage, frequency, etc can greatly reduce the number of adverse events arising from medication errors. Sharing this simple message across Ireland could make a real difference to addressing medication safety in our country — and can save lives.”
Patients and carers find lists useful in emergencies, when changing healthcare setting or provider, and to talk to healthcare professionals about medicines.“
Healthcare professionals find them useful to identify medication issues, increase patient awareness and contribute to safer and smoother transitions. At medical appointments, limited information may be available, and it may be relating to a single specialty, or organ only. Sharing a patient list may aid rapid and accurate communication and avoid duplication or interactions.
“This is a really great idea. Having a standard way to access a list of medications a person might be taking has several benefits. From a personal point of view, I often forget the names and doses of my meds so this would save a massive headache — currently, I save them in an online document (which takes me time to find), or I have to find out through my doctor’s surgery which is very slow, and a bit hit or miss. Certainly, nothing I think I could do quickly in an emergency.” Dave Milliken, Belfast
Patients and carers have identified community pharmacists and GPs as best placed to promote the use of a list. Promoting the use of the list is different to compiling the list for the patient, and wherever possible, the patient should be encouraged and empowered to create their own list.
Research has shown people like to use different formats for their list, including making the information compact and wallet-sized, taking photos of their medicines list or their medicines, or using a medicines app. The key is that people have a list, keep it updated and use it in appointments so the person and the healthcare professional have access to their medicines information.
The HSE National Medication Safety Programme has developed a blank medicines list template which patients can use to create their own medicines list. It has been designed to capture all the key bits of information that should be included on a medicines list. Blank My Medicines List leaflets are available to download at www.safermeds.ie. Hard copies can be ordered in boxes of 2,000, free of charge from www.healthpromotion.ie.
Patients may request a printout of their dispensed medications, and this can be a helpful tool in helping them to create their own full medication list. Where a patient requests a list, encourage them to add to it where relevant. They could also be prompted to transcribe the list onto the My Medicines List leaflet.
Throughout the month of April Patients for Patient Safety Ireland, the HSE National Medication Safety Programme and the IPU are encouraging pharmacy teams to engage with and encourage people to keep an up-to-date list of their medicines, and explain why it can be helpful. Some ideas to help in this process include:
An online training programme, Medication Without Harm, is available on www.iiop.ie or www.hseland.ie. Suitable for any member of the pharmacy team, the training helps you to understand medication related harm, and how to reduce it. It focusses particularly on working with patients to improve understanding and communication around medicines, including the use of a medicines list.
References available on request
Click here to download your Medicine list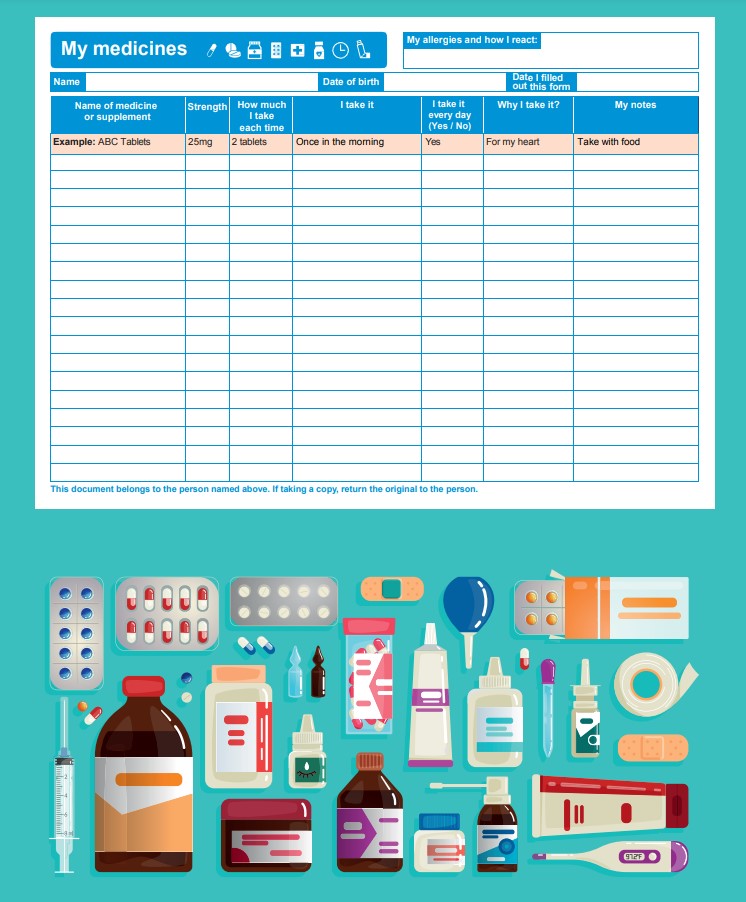
Having an up-to-date list of your medicines can help:
Make sure to keep a copy for yourself.
To fill out a My Medicines List you need all your medicines in front of you. Include all the medicines you take regularly and occasionally. All medicines count including:
Prescription medicines:
If you need help filling out your My Medicines list, you can ask for help, for example, from a family member or friend.
Bring this list with you when attending any healthcare appointment. This might include:

Do not assume your healthcare team member will have this information.
Changes to your medicines?
Ask your doctor, pharmacist or nurse to explain any changes to your medicines.
Patients for Patient Safety Ireland

the IPU and the HSE
Highlighted Articles