Home » IPU Medicine Shortages Survey 2025

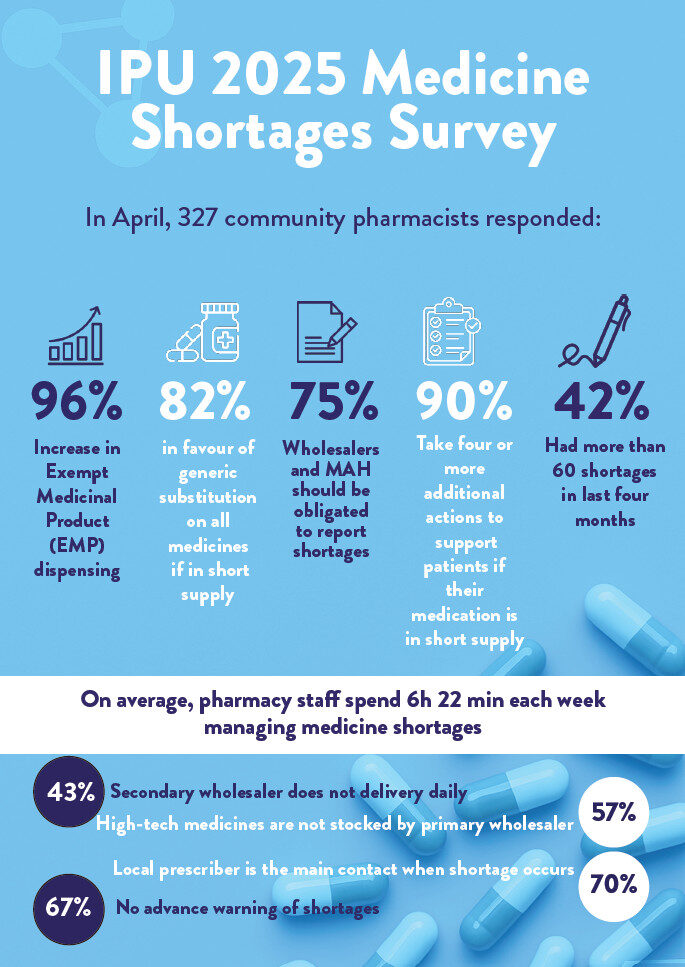
The IPU recently conducted its annual Medicine Shortages Survey for 2025, gathering important insights from pharmacists across Ireland. This year’s survey saw an increase in pharmacist participation compared to 2024, reflecting growing concerns within the pharmacy community on this critical issue. The survey results highlight the ongoing challenges faced by pharmacists in managing medicine shortages, the impact on patient care, and the extraordinary measures taken by pharmacists to mitigate these issues.
The IPU’s annual Medicine Shortages Survey was conducted between the second half of March and the first week of April this year with 327 responses received, which is an increase on last year’s survey. In this year’s survey, the questions were kept in a similar format to last year to gauge for emerging trends with shortages. The overall results of this year’s survey lean towards a levelling out of shortages encountered amongst pharmacists with 57 per cent saying that over the past 12 months medicine shortages have “significantly increased”, compared to 82 per cent in 2024. Additional fields were added to allow for a greater analysis of the number of shortages encountered by pharmacists over the last four months, but the overall total for the 41 or more medicines shortages remained at 57 per cent, which was equivalent to last year’s response.
Table 1: Approximately, how many shortages have you encountered in the last four months?
| 2017 | 2018 | 2019 | 2020 | 2023 | 2024 | 2025 | |
| None | 0% | 1% | 1% | 1% | 0% | 0% | 0% |
| 1-5 | 9% | 8% | 1% | 4% | 0% | 1% | 0.3% |
| 6-10 | 30% | 23% | 8% | 12% | 2% | 2% | 4% |
| 11-15 | 21% | 20% | 14% | 13% | 3% | 5% | 6% |
| 16-20 | 12% | 12% | 11% | 13% | 8% | 9% | 9% |
| 21-30 (or more) * | 28% | 36% | 65% | 57% | 14% | 13% | 14% |
| 31-40 | 13% | 14% | 11% | ||||
| 41-50 (over 41)** | 60% | 57% | 9% | ||||
| 51-60 | 6% | ||||||
| Over 61 or more | 42% |
(*please note additional fields were added in 2023 due to the large volume in the upper category — in surveys from 2017 to 2020, the last category was 20 or more)
(***please note additional fields were added in 2025 due to the large volume in the upper category — in surveys from 2023 to 2024, the last category was over 41)
When asked about their experience of medicine shortages over the last 12 months, Table 2 shows that pharmacists reported a downward trend, with 57 per cent saying medicine shortages have “significantly increased”, compared to 82 per cent of respondents last year. There has been an increase in the medicine shortages “somewhat increased”, and an increase in pharmacists reporting “no change”. On a slightly positive note, 2 per cent of pharmacists are reporting there has been a decrease in medicine shortages in the last 12 months which has not been encountered since 2020.
Table 2: In your opinion, over the past 12 months, have medicine shortages:
| 2017 | 2018 | 2019 | 2020 | 2023 | 2024 | 2025 | |
| Significantly Increased | 52% | 48% | 92% | 70% | 97% | 82% | 57% |
| Somewhat Increased | 38% | 40% | 7% | 27% | 3% | 15% | 32% |
| No Change | 9% | 11% | 1% | 2% | 0% | 3% | 9% |
| Decrease | 0% | 0% | 2% | 1% | 0% | 0% | 2% |
There is also a small glimmer of hope amongst pharmacists when asked to look to the future (see Table 3), with 78 per cent of the opinion that medicine shortages will increase in the next 12 months, which is slightly less than last year, but still not a very positive prediction as more pharmacists this year believe there will be no change.
Table 3: In your opinion, in the next 12 months, will medicine shortages:
| 2017 | 2018 | 2019 | 2020 | 2023 | 2024 | 2025 | |
| Increase | 86% | 84% | 92% | 92% | 87% | 84% | 78% |
| No Change | 14% | 16% | 6% | 7% | 11% | 16% | 21% |
| Decrease | 0% | 0% | 2% | 1% | 2% | 1% | 1% |
Political unrest, and future instability in global markets is another trend that emerged from the pharmacists’ responses. Many pharmacists have a keen awareness of the impact that world conflicts could have on the Irish market.
Changes in prescribing patterns were also cited as a reason for continuous medicine shortages. Everyone is aware of the media attention surrounding Ozempic and HRT medicines and the increase in prescriptions for same:
A notable theme that was highlighted in the 2023 Medicine Shortages Survey is also prevalent in this year’s, and that is around allocations and restrictions imposed by wholesalers. This is causing a lot of unease and unrest amongst pharmacists who believe that their patients are adversely affected with regards continuity of supply:
When asked if they struggle to get medicines which are not out of stock from wholesalers in a timely manner, even when they are not listed as out of stock at a country level, pharmacists replies were very similar to last year, with 80 per cent saying yes. Most pharmacists (95 per cent of respondents), indicated that this was due to products being on allocation, further cementing the quotes by pharmacists above. In line with last year’s results, the next highest reason was that High-Tech medicines were not stocked by the primary wholesaler (57 per cent, which is an increase from last year).
Pharmacists reported lack of communication on shortages as a major issue, and the sheer amount of time that is involved in having to continuously check if medicines are in stock in wholesalers. One pharmacist said, “On occasion, items may be listed as in stock on website but will not arrive. No communication from wholesaler as to why. Takes pharmacy staff to phone them only to be told they cannot supply”.
The average time spent per month by pharmacists/pharmacy staff in resolving medicines shortages remains like last year, as can be seen in Table 4. It is positive to see a slight downward trend, with 5 per cent less reporting that they spend 30 hours plus per month on this, compared to last year.
Table 4: What is the average time spent per month by you and/or other pharmacy staff in resolving medicine shortages?
| 2017 | 2018 | 2019 | 2020 | 2023 | 2024 | 2025 | |
| 0-5 hours | 27% | 25% | 16% | 17% | 7% | 4% | 4% |
| 5-10 hours | 48% | 50% | 34% | 40% | 25% | 19% | 24% |
| 10-20 hours | 17% | 18% | 30% | 29% | 26% | 34% | 34% |
| 20-30 hours | 5% | 5% | 9% | 7% | 18% | 18% | 18% |
| 30 hours plus | 3% | 2% | 11% | 7% | 23% | 25% | 20% |
To allow for comparison to European figures, pharmacists were asked once again this year how many hours they and/or other pharmacy staff spend dealing with medicine shortages per week. Irish pharmacists and pharmacy staff are spending six hours and 22 minutes per week managing medicine shortages. This is an increase on last year, where pharmacists and pharmacy staff were spending 4 hours and 37 minutes per week managing medicine shortages.
When faced with a medicine in short supply, pharmacists and their staff continuously go the extra mile to try and ensure continuity of supply and provide the utmost care for their patients. Table 5 highlights some of the measures that pharmacists take to ensure patient outcomes are not adversely impacted.
Table 5: Please indicate the measures you take to ensure patient outcomes are not adversely impacted when a medicine is in short supply (when medicine is not on the generic substitution list)?
| 2024 | 2025 | |
| Contact prescriber to suggest an alternative product | 98% | 95% |
| Source an Exempt Medicinal Product (EMP) | 96% | 95% |
| Borrow stock from another pharmacy for immediate patient need | 86% | 83% |
| Contact wholesalers for return date | 88% | 88% |
| Contact manufacturer for return date | 49% | 44% |
| Check the IPU shortages list | 49% | 49% |
| Check the HPRA shortages list | 55% | 52% |
| Other (please specify) | 14% | 13% |
These are labour-intensive tasks that happen quietly in the background, often unnoticed by patients, but essential to keeping the system running. There is no remuneration for this extra workload that pharmacists carry out. Indeed many pharmacies end up losing money as they source Exempt Medicinal Products (EMPs) for the sake of their patient, whilst being aware their patient is unable to afford to pay the additional cost that would be incurred. Pharmacists increasingly report that they frequently shoulder the financial impact to provide essential care for their patients.
One pharmacist replied, “paying for many ULMs (unlicensed medicines) out of our own pocket, due to lack of patient finance”.
“These are labour-intensive tasks that happen quietly in the background, often unnoticed by patients, but essential to keeping the system running. There is no remuneration for this extra workload that pharmacists carry out.”
The 13 per cent of pharmacists that replied ‘other’, cited the following measures to ensure patient outcomes are not adversely impacted:
When asked what the preferred method of communication to contact a prescriber was, 72 per cent of pharmacists indicated Healthmail, which is an increase from 58 per cent last year. It must be noted that many pharmacists in the comments section noted that even when sending a Healthmail, they must follow up with a phone call to the prescriber.
Others noted that in some instances the patient must return to the prescriber to aid in finding a solution; “It’s increasingly difficult to contact the prescriber. They don’t respond quickly to emails and impossible to get reply on phone. Sometimes you have to send patient back to prescriber. Not ideal.”
When asked if their patients’ health outcomes been adversely affected by medicine shortages, 71 per cent of pharmacists replied ‘yes’ (see Table 6). This is an increase on last year, and despite the phenomenal efforts of pharmacists and their GP colleagues to mitigate these issues by measures such as those listed in Table 5, shortages are still causing huge problems for patients. Some pharmacists reported that their patients ended up with a delay in treatment whilst trying to source the required medicine.
Pharmacists are reporting high anxiety levels among patients, with worry and distress also affecting patients, as well as unexpected financial burden:
Table 6: In your opinion, have your patients’ health outcomes been adversely affected by medicine shortages?
| 2017 | 2018 | 2019 | 2020 | 2023 | 2024 | 2025 | |
| Yes | 49% | 41% | 51% | 48% | 65% | 66% | 71% |
| No | 10% | 9% | 14% | 15% | 5% | 6% | 6% |
| Don’t Know | 41% | 50% | 35% | 37% | 30% | 28% | 22% |
The number of pharmacists who are signed up to receive alerts from the Health Products Regulatory Authority (HPRA) remained the same as last year, with just under half of respondents (49 per cent) signed up.
| 2020 | 2023 | 2024 | 2025 | |
| Yes | 52% | 35% | 47% | 26% |
| No | 48% | 65% | 53% | 33% |
| Not applicable, not signed up* | 41% |
(*Please note, this option was added for 2025 survey)
Table 7 depicts how useful pharmacists perceive the HPRA alerts on medicine shortages to be, with a reduction in pharmacists finding it useful in the last year. Reasons for not signing up to these alerts included pharmacists not being aware of same, and one pharmacist expressing frustration that, “There is no point in being alerted to shorts unless there is a realistic and agreed return date which we can depend on”.
Table 7: Have you found the alerts from the HPRA on medicine shortages useful?
| 2020 | 2023 | 2024 | 2025 | |
| Yes | 52% | 35% | 47% | 26% |
| No | 48% | 65% | 53% | 33% |
| Not applicable, not signed up* | 41% |
(*Please note, this option was added for 2025 survey)
Pharmacists believe that the three most common causes of shortages are allocation imposed by manufacturer (58 per cent), national pricing policies (55 per cent) and small market size — not economical to place the product on the market (54 per cent). This is in line with last year’s feedback which shows that pharmacists believe the reasons behind shortages is a long-term, multi factorial problem.
The number of pharmacists reporting medicine shortages on a regular basis has decreased since last year to 21 per cent. It is likely that pharmacists are fatigued with reporting shortages, with one pharmacist saying, “I’ve given up on reporting shortages. Surely it should be the job of the wholesalers to report them? There have been too many to report, I did it a lot at the start of the service, but I no longer do.”
Of the pharmacists that do report medicine shortages, the main channel of communication is with local prescribers, and shows a slight increase on last year, as can be seen in Table 8.
Table 8: If you ticked yes to the above question, who do you report shortages to? (tick any that apply)
| 2023 | 2024 | 2025 | |
| HPRA | 9% | 26% | 16% |
| IPU – Product File Team | 9% | 5% | 5% |
| Wholesaler | 40% | 21% | 30% |
| Local Prescribers | 71% | 66% | 70% |
| Pharmacy Head Office | 21% | 25% | 22% |
| Buying / Symbol Group Head Office | 16% | 13% | 16% |
| Other (please specify) | 11% | 8% | 7% |
The overwhelming majority of pharmacists believe that the responsibility for reporting medicine shortages should not fall on pharmacists. Instead, they believe this obligation should lie with wholesalers (76 per cent) and manufacturers (75 per cent). One pharmacist captured the general sentiment, stating, “Please do not suggest adding another admin task to pharmacists — this should be the obligation of the manufacturers/wholesalers”.
Pharmacists are striving for streamlined work processes and to provide the best patient care possible, and Table 9 indicates what solutions are favoured in the management of medicine shortages in Ireland, with an increased number in favour of generic substitution, and temporary reimbursement codes mentioned frequently in the comments; “Temporary codes being issued by PCRS to ensure pharmacist and patient not impacted financially”.
Table 9: What solutions would you favour in the management of medicine shortages in Ireland? (you may indicate more than one answer)
| 2023 | 2024 | 2025 | |
| Generic substitution on all medicines if in short supply (not just those on HPRA interchangeable list) | 67% | 78% | 82% |
| Preparing a compounded formulation | 5% | 4% | 3% |
| Importing the medicine from a country where it is available | 55% | 60% | 64% |
| Changing to the same medicine with a differing strength and adjusting the dose accordingly | 31% | 46% | 52% |
| Therapeutic substitution | 48% | 59% | 56% |
| Serious Shortage Protocol (Similar to the UK system) | 65% | 59% | 57% |
| Exportation ban of medicinal products that are in short supply in Ireland | 56% | 60% | 53% |
| Other (please specify) | 4% | 6% | 7% |
The number of EMPs dispensed by pharmacists has decreased slightly over the last 12 months but remains quite high, as can be seen in Table 10. Dispensing of EMPs is now a common everyday occurrence in pharmacies and bring with them an additional workload to the pharmacist. From sourcing the most cost-effective alternative, to counselling (especially challenging as many of the information leaflets and boxes are in different languages), to the burden of potentially trying to get this alternative covered under some of the community drugs schemes, with notable mention to the arduous and aptly named Hardship Arrangement.
Table 10: Has there been an increase in the number of Exempt Medicinal Products (unlicensed medicines) you dispense?
| 2017 | 2018 | 2019 | 2020 | 2023 | 2024 | 2025 | |
| Yes | 90% | 91% | 93% | 92% | 95% | 98% | 96% |
| No | 5% | 6% | 3% | 5% | 3% | 1% | 2% |
| Don’t know | 5% | 3% | 3% | 3% | 2% | 1% | 2% |
Pharmacists’ perception is that most patients do not have a clear understanding of what an EMP is, as can be seen in Table 11. It is only from the pharmacists spending time explaining and answering any questions that that may arise, that patients’ understanding deepens.
Table 11: What in your opinion is a patient understanding of an Exempt Medicinal Product (unlicensed medicines), when you are counselling them on the need for the use of this product(s)?
| 2024 | 2025 | |
| Good, they understand that the medicine is licensed in another country and just not available in Ireland | 10% | 11% |
| Fair, they understand it is the same medicine, just sourced from a different country | 36% | 37% |
| Unaware, they would not have a good understanding of what an exempt medicinal product is | 52% | 49% |
| Other (please specify) | 2% | 3% |
An alarming trend in the responses in this year’s survey is the increased workload and burden that pharmacists are experiencing day-in, day-out, with no apparent end in sight. One pharmacist reported, “It’s escalating at an outrageous rate. It’s impacting on patient care and the mental health of pharmacy staff.” Another pharmacist gave a gruelling insight into their workday:
“It’s just relentless, every day there are new shortages and it just seems when one thing comes back something else is gone — changing brands on patients all the time, no consistency, having to change labels, run something through, then go to the shelf, it’s not there, why not, gone out of stock, go back to the computer, change the label to a different brand if available, if not contact patient, see how many they have left, have we a few days grace to see if stock comes in, do we need to borrow, ring around other their pharmacies, before contacting doctor for a change of prescription. I am drained just writing this down, and this happens so many times during the working day.”
The IPU NHPC Medicines Shortages List monitors shortages of Irish licensed medicines and provides information on re-supply dates together with information on any alternatives that may be available.
The IPU NHPC receives details of medicinal product shortages from a variety of stakeholders including the HPRA, manufacturers, wholesale distributors, marketing authorisation holders, IPU members and the HSE. Shortages can be logged on the IPU NHPC database. The IPU NHPC follows up with stakeholders regularly to update re-supply dates and include details of resolved shortages, as necessary.
Analysis of the IPU website user information indicates the Medicine Shortages page is the most visited page of the website (see ipu.ie > Members Support > IPU Product File > Medicines Shortages Update).
Noelle Horan

Medicines Information Pharmacist, IPU
Highlighted Articles