Home » About allergic rhinitis

Allergic rhinitis (AR) refers to inflammation of the nasal passages, which results in symptoms such as sneezing, nasal congestion, itchy nose and blockage. Rhinitis, which is caused by an allergic trigger, is known as Allergic rhinitis. This accounts for about 75 per cent of rhinitis cases, while the remaining 25 per cent are caused by non-allergic rhinitis. It is estimated that over 80 per cent of people with asthma have AR. In addition, one in five of the general population are affected by AR (HSE: Overview on Allergic Rhinitis, available at hse.ie). It is also a risk factor for asthma, with 10 – 40 per cent of people who have AR also having asthma. AR is more likely to develop initially, with asthma developing later. Therefore, people with AR that develop asthma symptoms should be formally assessed. Similarly, patients with persistent asthma should be evaluated for AR. As spring and summer emerge, this can be a challenging time as various pollen levels start to increase.
AR and asthma often coexist as “united airway disease” or “one airway disease”. Both conditions are chronic inflammatory diseases affecting the upper and lower airways. They can be triggered by allergic or non-allergic triggers and may present as several phenotypes. Assessment and management of AR and asthma should be jointly carried out, leading to better control of both conditions.
Rhinitis can occur without a known allergic trigger, which is known as non-allergic rhinitis (non-AR). Non-AR accounts for about 25 per cent of rhinitis cases. Non-allergic rhinitis can be caused by structural nasal problems such as septal deviation and exposure to environmental pollution, chlorinated pools, and even fragrances. Hormonal changes that occur during puberty, pregnancy, and menopause can also act as a trigger. Other triggers can include spicy foods and weather changes and overuse of nasal decongestant sprays.
Typical symptoms of seasonal (Hayfever) and perennial allergic rhinitis are:
Patients may experience all or some of the above. Symptoms may also be confused with symptoms of COVID-19.
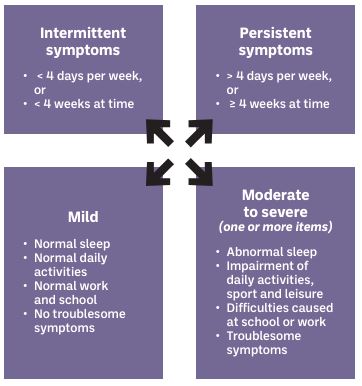
In 2019, the classification of “seasonal” and “perennial” rhinitis was changed to “intermittent” and “persistent” rhinitis. Intermittent rhinitis occurs less than four days per week or for less than four weeks. Persistent rhinitis lasts more than four days per week and longer than four weeks. Both intermittent and persistent AR can be mild or moderate/severe (see Figure 1).
Figure 1: Classification of allergic rhinitis (ARIA, 2019)
There are several treatment options available to the patient and a combination of these options may be required for optimal relief of symptoms. These are outlined in Table 1. Saline douching/nasal irrigation should also be encouraged, and is available either as a saline rinse or saline spray. Saline rinsing involves high volume at low pressure, whereas saline spray is a low volume delivered at high pressure. The advantages of saline douching include:
Smoking and vaping cessation should be encouraged at every opportunity. Smoking and vaping may increase the likelihood of chronic nasal symptoms.
Table 1: Pharmacological options for allergic rhinitis
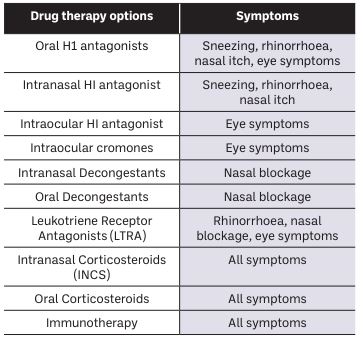
Figure 2: Using a nasal spray
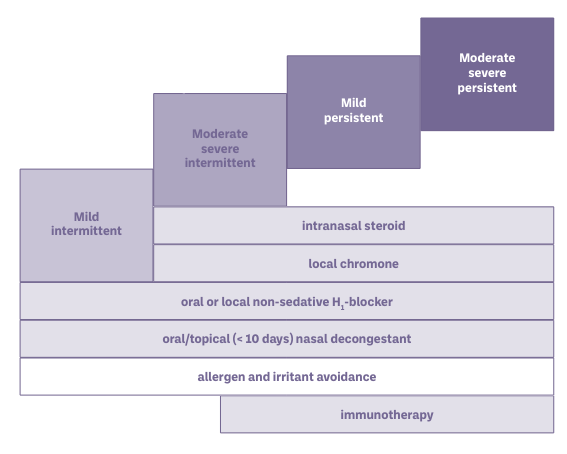
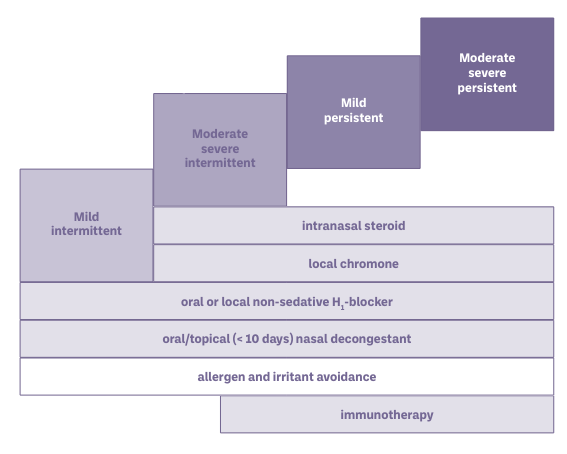
Mild intermittent AR treatment options include oral and nasal decongestants, which can be used as a rescue medication. These medications will reduce nasal congestion and should be used for no longer than seven days. They should also be avoided during pregnancy and breastfeeding. Oral H1 antagonists block the physiological effects from mast cell-derived histamine. Second generation antihistamines are preferred due to their less sedating effect and most are available over the counter. Intranasal and intraocular antihistamines are also available. Intranasal corticosteroid (INCS) is the first- line treatment for moderate/severe intermittent and persistent AR. These medications are used once or twice daily to each nostril, and good technique is essential. It should be checked at every opportunity. If the nasal cavity is very obstructed, a nasal spray may not be effective. Nasal drops may be more effective in this scenario. Nasal spray and nasal drop technique can be viewed at asthma.ie > About us > Resources.
The efficacy of INCS is not improved when used with oral corticosteroids (OCS). Figure 3 provides a stepwise approach to the management of AR.
Immunotherapy is also recommended by ARIA (2019) for patients with AR who do not achieve an optimal response from oral H1 or INCS therapies. Sublingual Immunotherapy (SLIT) to house dust mite is now recommended by the Global Initiative for Asthma (GINA, 2023). Some of these treatments are available on the GMS and can be prescribed by GPs. There are three SLIT/AIT products available in Ireland to treat allergy — grass pollen, tree pollen, and house dust mite allergy.
Figure 3: Stepwise pharmacological treatment for allergic rhinitis
Endonasal phototherapy is not commonly used as a treatment in Ireland and is not recommended by GINA or ARIA. There is some evidence to suggest that phototherapy is an effective treatment in improving nasal symptoms scores triggered by AR. Endonasal phototherapy has an immunosuppressive effect by inhibiting allergen-induced histamine released from mast cells. It also induces apoptosis in T-lymphocytes and eosinophils. The procedure directs a combination of UV-B, UV-A, and visible light into the nasal cavity.
It is considered that allergic rhinitis is a medical condition that requires medical intervention. However, if symptoms are unilateral or if there is a septal deviation, nasal polyps or tumour present, surgery should be considered. Patients will still need to have an AR plan in place post-surgical intervention.
Walker et al showed that allergic rhinitis can have a significant impact on exam performance and results, with students dropping a grade in the state exams compared with their mock exams. Students should be advised to have their allergic rhinitis assessed and treatment started well in advance of sitting exams, usually around Easter time. Some other useful tips during exam time include:
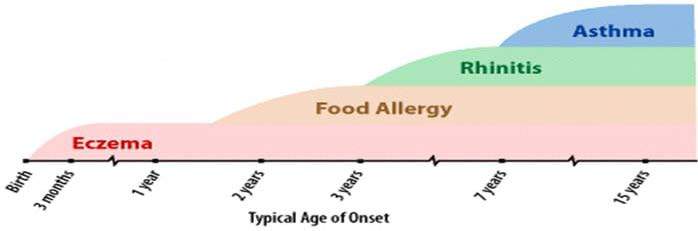
Figure 4 illustrates the typical age at which allergies are onset in children. Outdoor allergens are unusual in children under two years of age. Type 2 sub-endotype IL4/IL-13 are associated with AR in children. IL-5 is associated with asthma. Treatment of children under four should focus on allergen avoidance and saline spray. Cetirizine is the oral H1 antagonist of choice. Cetirizine is licensed from two years, but good safety is reported from six months of age. For moderate/severe persistent AR, intranasal corticosteroids such as Fluticasone or Mometasone should be considered first line treatment. Long-term follow-up studies suggest no growth retardation if used as a once-daily dose. Caution should be taken in children who are also using inhaled or topical corticosteroids for asthma or dermatitis. In children with resistant symptoms and those with co-existing asthma, leukotriene receptor antagonists should be considered. Parents should be educated about the possible side effects of sleep disturbance and mood disorders.
Figure 4: The Allergic March in Children
AR affects 20% of pregnancies, and women with pre-existing AR can experience an increase in symptoms. Medications and immunotherapy for AR are used under a doctor’s supervision. Oral decongestants should be avoided. It is important that patients consult their doctors before taking any medication during pregnancy. For allergic rhinitis nasal anti-histamines, with or without steroids, are safer and often more effective than tablet equivalents.
This article has explored the assessment and management of AR. Special considerations in children and pregnancy have also been addressed. The impact of allergic rhinitis on health and wellbeing is significant, with many people experiencing impairment of daily activities, learning and cognitive function, and reduced productivity at work and school. Optimal control of symptoms through pharmacological and non-pharmacological treatment regimes in combination with education, self-management and empowerment is paramount to managing this distressing condition.
People with questions about managing their asthma are encouraged to send a WhatsApp message to the HSE-funded Asthma WhatsApp service on 086 059 0132 or Freephone the Asthma Society’s HSE-funded Asthma Adviceline on 1800 44 54 64. Both services are free and allow users to communicate directly with an asthma nurse specialist (Figure 5).
To support pharmacists this hay fever season, the Asthma Society of Ireland has recently launched its new e-referral platform for healthcare professionals.
The platform, available at asthma.ie/patient-e-referral, allows healthcare professionals all over Ireland to refer patients or carers with questions or concerns about asthma or COPD to the charity’s Adviceline and WhatsApp services.
For more information about hay fever and to access the Asthma Society’s resources visit asthma.ie.
The Asthma Society’s Hay Fever Campaign is kindly supported by ALK.
References are available on request
Thank you to members of the Asthma Society of Ireland’s Medical Advisory Group, including Respiratory Nurse Specialists Johanna O Callaghan, Paula Hallahan, and Professor Marcus Butler, for peer reviewing this article.
Ruth Morrow

Respiratory Nurse Specialist, the Asthma Society of Ireland
Highlighted Articles