
The information provided was valid at the time of the publication of this CPD article.
The COVID-19 pandemic has further highlighted the importance of helping smokers to quit. Now, more than ever, the most significant single step a smoker can take to improve their health is to stop smoking. However, a successful quit attempt often requires more than knowledge and motivation. Quit attempts are most effective when accompanied by tailored, timely and empathetic support and pharmacological aids.

Despite much progress, in 2020, 15.4% of Irish people over 15 years still smoke. A further 5.8% use e-cigarettes. While evidence shows that patients expect to be asked questions by their health professional about their lifestyle, if they are not asked, they assume that there is not a problem.
In one Healthy Ireland study, only 38% of Irish smokers who attended a health professional in the preceding year reported that the health professional had discussed quitting smoking with them, while 62% missed the opportunity to ‘Make Every Contact Count’.
Pharmacy teams have millions of contacts each year with patients. These are all potential opportunities to empower and support them to make healthier choices, such as to stop smoking. So how can we be optimally effective in supporting smokers to quit?
The aim of this article is to show you how you can leverage your expertise in smoking cessation products, along with developing consultation skill mastery to increase the number of your patients who quit for good.
Remember: Supporting patients to quit smoking is life-saving work. One in every two smokers will die from a tobacco related disease and most smokers lose between 10 to 15 quality life years.
At the end of this article, you will be able to:
Healthcare professionals usually prioritise the health benefits of quitting. However, many smokers may be more motivated to quit by other wellbeing benefits. (Table 1).
| Within 20 minutes | Blood pressure and pulse rate return to normal |
| Within 8 hours | Oxygen levels return to normal. |
| Within 24 hours | Carbon monoxide is eliminated from the body. Mucus in the lungs begins to clear |
| After 48 hours | Smell and taste are enhanced |
| In 72 hours | Breathing becomes easier. Energy levels increase |
| After 2 weeks | Circulation improves |
| Longer Term Health Benefits of Stopping Smoking | |
| After 3-9 months | Coughing, shortness of breath and wheezing are reduced dramatically. Chest infections and colds become less frequent. |
| After 5 years | Risk of heart attack falls to that of a non-smoker. |
| After 10-15 years | Risk of lung cancer falls to half that of a non-smoker. |
| Other Wellbeing Benefits of Stopping Smoking | |
| Financial | Reduced cost of life insurance, dental and medical bills. The average smoker, smoking 20 cigarettes per day can save €4,380 per year on the cost of cigarettes alone |
| Appearance | Reduced staining of teeth. Reduced wrinkles. |
| Quality of Life | Gain 10-15 quality life years. |
| Emotional | Improved positive mood and quality of life. Reduced depression, anxiety and stress. |
| Social | Being a non-smoker is more social. Exposing other people to passive smoking is considered anti-social. |
| Environmental | Better air quality. Nicer smelling clothes. |
| Role Model | Improve the health of loved-ones through role-modelling and reduced smoke exposure. |
Table 1: Immediate Health Benefits of Stopping Smoking
There are three key factors that influence why people may continue to smoke, even when they want to quit. How these factors interplay is different for each smoker. To offer the most appropriate and effective smoking cessation support, you must first help the person understand the degree to which each factor is at play for them.
The Fagerstrom Test is a six-question survey to help you determine their level of nicotine dependence. Indicators that a smoker may have a high level of nicotine dependence include smoking soon after waking and smoking more than 20 cigarettes per day.
Smoking Cessation Pharmacotherapies can play a primary role in supporting a person with a high physical dependence to quit. POM varenicline, NRT 24hr patches and NRT 16hr patches + a quick release NRT formulation are often effective choices. High dose NRT and varenicline have been shown to have similar abstinence rates after six months, but varenicline shows superior abstinence rates as a monotherapy after one, three and 12 months.
Smoking is often associated with and reinforced by routine activities, people and situations e.g. at the end of a meal or driving the car. For some people, the feel, smell and sight of a cigarette and the ritual of handling, lighting and smoking it, are all part of the enjoyment and pleasure of smoking. Within a short time, smoking becomes an unconscious habit, that is continually reinforced. For example, a 20/day smoker typically makes the hand to mouth movement 200 times per day (73,000 per year!).
Smoking Cessation Pharmacotherapies that tend to be most effective for smokers with a high behavioural dependency include NRT inhalator or NRT gum. The inhalator replicates the hand to mouth action of smoking. The gum offers an alternative behaviour (chewing). For patients with both a high physical and behavioural dependence, a combination of NRT Patch + NRT inhalator or gum can be useful.
Smoking is often used as an aid to manage stress and negative feelings of anxiety, frustration or anger. However, because nicotine is a stimulant it doesn’t actually help a person relax. Many smokers use smoking rituals to give structure to their daily routine by providing breaks. Smoking is sometimes used to convey confidence or as an ice-breaker in social situations.
For people with primarily psychological dependence, pharmacotherapies tend to play a more supportive role in smoking cessation. In addition to NRT or varenicline to help manage nicotine cravings, it is important to help the person identify the needs that are being met by smoking e.g. “I need to relax,” and explore alternative ways to meet those needs e.g. relax by deep breathing (without a cigarette), distraction or mindfully drinking a glass of water.
Quit rates are enhanced when supported by a supportive environment and development of alternative coping strategies. For this reason, patients should be sign-posted to the HSE Smoking Cessation Service:
The STEPS Consultation Framework provides a framework to build confidence and mastery in hosting these potentially life-saving consultations.
| Stage of Change | You might hear |
| Pre-contemplation (no intention of quitting in the next six months) | I won’t / I can’t |
| Contemplation (intends to take action in the next six months) | I might/ I’d like to |
| Preparation (intends to take action in the next 30 days) | I will |
| Action (has changed overt behaviour for less than six months) | I am |
| Maintenance (has changed overt behaviour for less than six months) | I still am |
| Relapse | Negative self-talk |
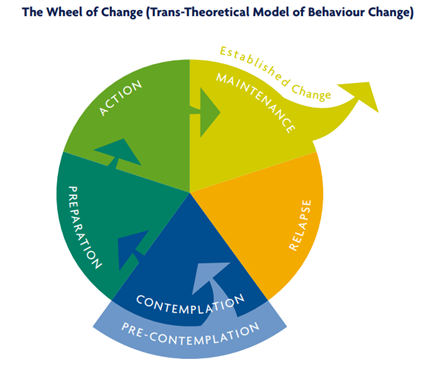
Research indicates that 59% of smokers are trying to (Action), planning to (Preparation) or thinking about (Contemplation) quitting.
“Supporting patients to quit smoking is life-saving work. One in every two smokers will die from a tobacco related disease and most smokers lose between 10 to 15 quality life years.”
Rachel Dungan

Share This Page