
The information provided was valid at the time of the publication of this CPD article.
Plaque psoriasis is a common, chronic, immune mediated condition that involves the skin and nails. Psoriasis vulgaris, or chronic plaque psoriasis, is the most common form of the disease, comprising 85-90% of cases. Psoriasis is characterised by the presence of symmetrically distributed, red, well-defined plaques with a silvery surface scale. The scale is usually silvery white.
Although any part of the skin can be affected by psoriasis, it most commonly occurs on extensor surfaces and scalp involvement is common. Evidence suggests that there is a strong genetic component with 40-50% of patients having a family history of psoriasis. The basis for disease development is thought to be a complex interplay of genetic and environmental factors. Triggers include stress, trauma, smoking and alcohol.

Plaque psoriasis most commonly appears on elbows, knees, scalp and lower back but can appear anywhere on the body. The plaques can be itchy or sore, or both. In severe cases, the skin around joints may crack and bleed.
This has a huge negative impact on the lives of patients and can compound the low mood and feelings of distress and frustration with the condition.

Figure 1: Plaque Psoriasis (DermNet NZ)
This can occur on parts of your scalp or on the whole scalp. It causes red patches of skin covered in thick, silvery-white scales. Some people find scalp psoriasis itchy, while others have no discomfort. In extreme cases, it can cause hair loss, although this is usually only temporary.

Figure 2: Scalp Psoriasis (DermNet NZ)
In about half of all people with psoriasis, the condition affects the nails. Psoriasis can cause your nails to develop tiny dents or pits. They can become discoloured or grow abnormally. Nails can often become loose and separate from the nail bed. In severe cases, nails may crumble.
Guttate psoriasis causes small drop-shaped sores on your chest, arms, legs and scalp. There’s a good chance guttate psoriasis will disappear completely after a few weeks but some people go on to develop plaque psoriasis. This type of psoriasis sometimes occurs after a streptococcal throat infection and is more common among children and teenagers.
This affects folds or creases in your skin and appears in areas such as the armpits, groin, between the buttocks and under the breasts. It can cause large, smooth red patches in some or all these areas.
Inverse psoriasis is made worse by friction and sweating. This can be particularly uncomfortable in hot weather.
Psoriasis does not just affect the skin – it is a lifelong, serious immune-mediated condition. The PSO report, published in 2017, highlighted the debilitating effect psoriasis can have on emotional and mental wellbeing, as well as physical health.
As pharmacists we often see patients presenting to the pharmacy more frequently than to the GP. On a practical level, patients often present looking for emollients, topical steroids, creams and shampoos, sometimes with very little improvement of their psoriasis. Pharmacists can hear patients saying that they have tried everything and are now disengaging from treatment as ‘nothing has worked’ for them. It can affect their quality of sleep and can cause patients to cease or limit social activities they once enjoyed out of embarrassment or discomfort from the condition.
| Physical impact |
|
| Psychosocial impact |
|
| Socio-economic impact |
|
Table 1: The burden of psoriasis
A wide range of treatments are available for psoriasis. Identifying the most effective one can be difficult. It is important to encourage our patients to talk to their doctor if they feel a treatment is not working or if they have uncomfortable side effects.
| 1 | Topical Treatments come in the form of creams, ointments, lotions, gels, foam or mousse which are applied directly to the skin. |
| 2 | Phototherapy is a form of artificial ultraviolet light, delivered in hospital dermatology departments. |
| 3 | Systematic Treatments are drugs that work throughout the body. They may come in the form of a liquid, tablet or injection. |
| 4 | Biologic Treatments are targeted medicines used to inhibit part of the immune system that drive inflammation. These are mainly injections but some are now being developed in tablet form. |
Table 2: Daily Care and Treatments for Psoriasis
Topical therapy is first line treatment.
Topical options such as emollients, corticosteroids, coal tar preparations, and vitamin D analogues.
Emollients are widely used in psoriasis. They moisturise dry skin, reduce scaling and relieve itching. They also soften cracked areas and help other topical treatments absorb through the skin to work more effectively.
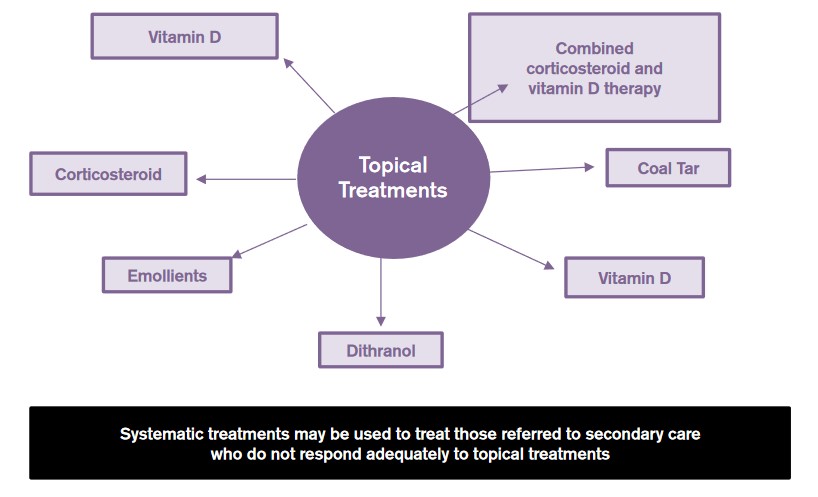
Figure 3: Key treatments in primary care.
These drugs are the most frequently prescribed medications for treating mild to moderate psoriasis. They are available as ointments, creams, lotions, gels, foams, sprays and shampoos. Mild corticosteroid ointments (hydrocortisone) are usually recommended for sensitive areas such as face or skin folds and for treating widespread patches. Other frequently prescribed corticosteroids are Betacap®, Betnovate® and Bettamousse®.
Vitamin D analogues
Calcipotriol – Dovonex® is a topical form of synthetic vitamin D with efficacy similar to that of moderate strength corticosteroids but with fewer of their potential side effects e.g. thinning of the skin. Dovonex® helps to normalise some of the irregular cell changes in psoriasis. It has no smell and is easy to use. It can be irritating at certain sites, is not recommended on the face and the maximum dose must not be exceeded.
Coal Tar
Coal tar reduces scaling, itching and inflammation. It is thought to work by decreasing the accelerated rate at which skin cells are produced in psoriasis. It’s available over the counter or by prescription in various forms such as shampoo, cream and oil. These products can irritate the skin. They’re also messy, stain clothing and bedding, and can have a strong odour. Coal tar products are not recommended for women who are pregnant or breast-feeding.
Calcineurin inhibitors
Calcineurin inhibitors such as tacrolimus (Protopic®) reduce inflammation and plaque build up. They can be especially helpful in areas of thin skin such as around the eyes where steroid creams or retinoids are too irritating or may cause harmful effects. If prescribed for the face, it is important to remind patients to apply a high SPF and minimise exposure to sunlight. Other forms of ultraviolet light treatment or sunbeds must be avoided. Stinging on application is the most common side effect but this usually settles within a few days. Protopic® should not be applied to infected skin. Calcineurin inhibitors are not recommended when pregnant or breastfeeding or if the patient intends to become pregnant. It is not intended for long term use because of a potential increased risk of skin cancer and lymphoma.
Salicylic acid
Salicylic acid shampoos and scalp solutions reduce the scaling of scalp psoriasis. It may be used alone or to enhance the ability of other medications to more easily penetrate the skin.
Phototherapy is a first-line treatment for moderate to severe psoriasis, either alone or in combination with medication. Repeated treatments are necessary.
Methotrexate
Usually administered weekly as a single oral dose, methotrexate decreases the production of skin cells and suppresses inflammation. It’s less effective than adalimumab (Humira®) and infliximab (Remicade®). It might cause upset stomach, loss of appetite and fatigue. People taking methotrexate long term need ongoing testing to monitor their blood counts and liver function.
Men and women should stop taking methotrexate at least three months before attempting to conceive. This drug is not recommended when breastfeeding.
Biologics. These drugs, usually administered by injection, alter the immune system in a way that disrupts the disease cycle and improves symptoms and signs of disease within weeks. Several of these drugs are approved for the treatment of moderate to severe psoriasis in people who haven’t responded to first-line therapies. The therapeutic options are rapidly expanding. Examples include etanercept (Enbrel®), infliximab (Remicade®), adalimumab (Humira®), ustekinumab (Stelara®), secukinumab (Cosentyx®).
Biologics must be used with caution because they carry the risk of suppressing the immune system in ways that increase risk of serious infections. Oral apremilast (Otezla®) is taken by mouth twice a day. It’s especially effective at reducing itching.
A focus on first line topical treatment:
Different types of topical treatments may be prescribed to be used in sequence e.g. topical corticosteroids may be used in addition to tar preparations or vitamin D analogues, with one applied in the morning and one in the evening. Patients can also be prescribed products that contain two topicals combined e.g. corticosteroid/tar mixtures, or the combination product betamethasone / calcipotriol (e.g. Dovobet® or Enstilar®) which contains both a potent (strong) corticosteroid and Vitamin D analogue, and which has the advantage of once daily application. Once a day application burden can dramatically increase patient adherence and positive outcome. The burden of twice daily applications of separate creams/gels can be a barrier in itself to adherence and therefore positive outcomes. Some ointments and gels may also negatively impact patients due to their consistency and sticky nature.

Figure 4: Reasons suggested for poor adherence
A potent topical steroid with vitamin D analogue.
Enstilar® is licensed as a flare treatment; once-daily, four week topical fixed dose combination treatment for plaque psoriasis of the body and scalp in adults. Patients who have responded at four weeks’ treatment are suitable for long-term maintenance treatment, which is twice weekly application. The spray application makes it easy for application in hard to reach places, like the back, for patients. Many patients live on their own so accessing hard to reach places easily is a consideration with the spray.
Enstilar® should be sprayed with the nozzle fully pressed down for two seconds for every hand sized plaque. A thin layer should be applied then gently rubbed in so all affected skin is covered. Wash hands well post application.
Dovobet® and Enstilar® combination products and can be used to treat scalp psoriasis.
Comb the hair to remove loose scales, apply products to the hand and use fingers to apply the products directly to the affected areas. Patients should try and minimise the amount applied to the hair to make it easier to wash out. Gently rub the foam into the scalp. The treatment should be left on the scalp over night or during the day.
It can be easier to remove products when shampoo is applied to dry hair as water dilutes the cleansing effect of the shampoo. Massage the shampoo into dry hair/scalp and leave for a few minutes before washing. A mild non-medicated shampoo should be used.
Topical tar preparation such as Cocois® can be effective at softening and removing scale. Usually, the tar is left in contact with the scalp for approximately one hour and then washed out with normal shampoo. Coal Tar can stain clothes and bedclothes so when leaving on overnight, pharmacists can suggest old pillow cases or shower caps to protect bedclothes from staining and it also helps the treatment to penetrate the scale. Cocois® should be used daily initially and then according to need.
Pharmacists are uniquely placed to help give practical advice for psoriasis sufferers and ensure the best outcome for their patients. It is pivotal for patients to know how to apply, how much and when to apply, where they can apply it and even how to wash it off, along with managing expectations of results. Topical treatments are first line treatments for adults and children. Correct application of topical treatments is key for positive outcomes.
Poor patient adherence to treatment and increase in anxiety levels during a flare up are commonly seen in practice. Erratic and inconsistent use of topical therapies can also compound a patient’s psoriasis.
Pharmacists working in a patient facing capacity across all sectors are trained to support patients with using medications effectively and provide solutions when patients encounter problems. Pharmacists can support the patient with advice which can help improve outcomes and safety for patients while helping to reduce waste.
Evidence suggests that a lack of response to treatment can be as much to do with poor adherence as it is to do with poor efficacy.
A topical combination product that can treat in a short period of time and lead to very good results helps patients to feel empowered and self-manage their condition successfully. Corticosteroids and vitamin D analogues complement each other in treating the key pathogenic factors of plaque psoriasis – skin proliferation and inflammation.
Combination products can reduce the application burden for the patient and improve application adherence and therefore outcome.
References available upon request.
Victoria Jones

Share This Page