Home » Lithium Therapy: a national patient safety and quality improvement initiative
The national patient information booklet on lithium therapy has been produced and updated by Audrey Purcell, Chief 2 Pharmacist, and the Saint John of God University Hospital Drug and Therapeutics Committee. The updated booklet will be launched this month and copies of it have been sent to pharmacies with this issue of the IPU Review. In this article, Ms Purcell provides an overview of the booklet.

The national patient information booklet has been produced and updated by Audrey Purcell, Chief 2 Pharmacist and the Saint John of God University Hospital Drug and Therapeutics Committee.
Image 1: Baseline work-up
Starting dose may usually range from 400mg-800mg OD (nocte) in adults, depending on indication. Elderly patients, those with renal impairment or those below 50kg in weight, often require lower starting dose (for example, 200mg), and maintenance doses.
Table 1: Lithium products| Product: | Formulation: | Recommended dosing: | Lithium level sampling time: |
| Priadel Tablets: 200mg+400mg (200mg tablet may be halved to facilitate 100mg dose) | Lithium Carbonate. | Once daily: at night (Prolonged Release) | 12 hours post dose (acceptable 10-14 hours) |
| Camcolit tablet EMP 400mg EMP: Exempt Medicinal Product | Lithium Carbonate | Once daily: at night (Prolonged Release) | 12 hours post dose (acceptable 10-14 hours) |
| Priadel Liquid EMP 520mg/5ml | Lithium Citrate 520mg/5ml: Equivalent to Lithium Carbonate 204mg/5ml (Use Carbonate 200mg=5ml for calculations) | Once daily: at night Twice daily: morning and night (Immediate Release) | Once daily: 12 hours post dose Twice daily: 12 hours post dose and sample to be taken pre-morning dose (acceptable 10-14 hours) |
| Li-Liquid EMP 509mg/5ml | Lithium Citrate 509mg/5ml: Equivalent to Lithium Carbonate 200mg/5ml (Use Carbonate 200mg=5ml for calculations ) | Once daily: at night Twice daily: morning and night (Immediate Release) | Once daily: 12 hours post dose Twice daily: 12 hours post dose and sample to be taken pre-morning dose (acceptable 10-14 hours) |
Priadel tablets are recommended for routine use. The 200mg tablets have score-lines, therefore they can be divided accurately to provide 100mg dosage requirements. If a patient is unable to swallow tablets a liquid may be prescribed, if essential. Particular care is required with lithium liquid as this can be associated with calculation and administration errors. It is essential that a switch from tablets to liquid is prescribed by the doctor, calculation confirmed by pharmacist, and clear dosage instructions provided to patient by the pharmacist.
Example: Switching patient from Priadel tablet (Carbonate) 800mg nocte to Priadel liquid nocte:
Lithium plasma level should be checked five to seven days after starting, after every dose change, and after addition/discontinuation of medication that can affect level.
The minimum effective plasma level for prophylaxis in adults is 0.4mmol/L; optimal range is 0.6-0.8 mmol/L. A level of 0.4mmol/L may be effective in unipolar depression; 0.6 -1 mmol/L in Bipolar Disorder, and levels at the higher end of the range in mania (0.8-1mmol/L).
TFTs, renal function, calcium level, and weight check, recommended every six months; or every three months in at-risk patients.
Once stable, serum lithium levels recommended every three months for the first year, then every six months; or every three months in at-risk patients.
At-risk patients include:
If a decision is made to discontinue lithium, the risk of relapse may be reduced by reducing the dose gradually. It is recommended to reduce the dose slowly over at least 4 weeks or longer, and preferably up to 3 months in Bipolar Disorder; except in medical emergency or overdose.
Table 2: ALARM bell medication interactions — think “ANTS”| Name: | Magnitude: | Timescale: | Additional Information: |
| A: ACE Inhibitors (ACEI) Angiotensin Receptor Blockers (ARBs) | Unpredictable. Up to four-fold increase in lithium level. | · Develops over several weeks; and · Most likely to cause lithium toxicity within a month of starting. | · Sevenfold increased risk of hospitalisation for lithium toxicity in the elderly; · Consider alternative anti-hypertensive; and · If combination necessary, increased monitoring of lithium level and renal function required. |
| N: Non- Steroidal Anti-inflammatories (NSAIDs) | Unpredictable From 10% to more than four-fold increase in lithium level. | · Variable: a few days to several months. | · Examples of increased lithium levels with oral NSAIDs include ( but are not limited to): up to 23% increase in lithium level with Diclofenac; up to 25% increase in lithium level with Ibuprofen; and · Patients should be advised to avoid oral OTC NSAIDs (examples include Ibuprofen) and use Paracetamol if OTC analgesic required. Pharmacist should contact doctor if oral NSAID prescribed with lithium. |
| T: Thiazide Diuretics | Unpredictable. Up to four-fold increase in lithium level. | · Thiazides reduce renal clearance of lithium and levels can rise within a few days; · Usually apparent in the first 10 days; and · Any effect will be apparent in the first month. | · Thiazide diuretics should only be used where unavoidable and with strict monitoring; and · Loop diuretics may be safer. Furosemide is the safest diuretic to use with lithium, but frequent monitoring required. |
| S: Sodium | Excess Sodium can reduce lithium levels. Sodium restriction can lead to lithium toxicity. | · Variable | · Consider high Sodium content OTC preparations and recommend suitable alternatives; · Care with Sodium content in effervescent formulations; and · Refer to SPS Pharmacy NHS Considering Sodium content of medicines; particular care with products > 17mmol Sodium in maximum daily dose. High-alert examples: (not an exhaustive list) 1) Sodium Bicarbonate in antacids (for example, Gaviscon): recommend Maalox instead; 2) High Sodium content in urinary alkalinising agents (eg Cymalon): avoid; and 3) High Sodium content in soluble/effervescent products: recommend film-coated tablets. |
The below is not an exhaustive list.
Cardiac: Lithium may cause cardiac arrhythmia, including bradycardia, sinoatrial dysfunction (SA block), abnormal T waves on ECG (T-wave inversion), and ST-segment depression.
Dermatological: Lithium may cause acne vulgaris and/or psoriasis (including exacerbation of both) in patients with and without either condition at baseline.
GI: Lithium may cause dyspepsia, diarrhoea, nausea, vomiting, dysgeusia (metallic or salty taste), gastritis and abdominal pain. Some effects (for example, nausea) may occur early in treatment. Other effects may take longer to develop. Supratherapeutic lithium levels should be suspected with severe nausea, vomiting and diarrhoea.
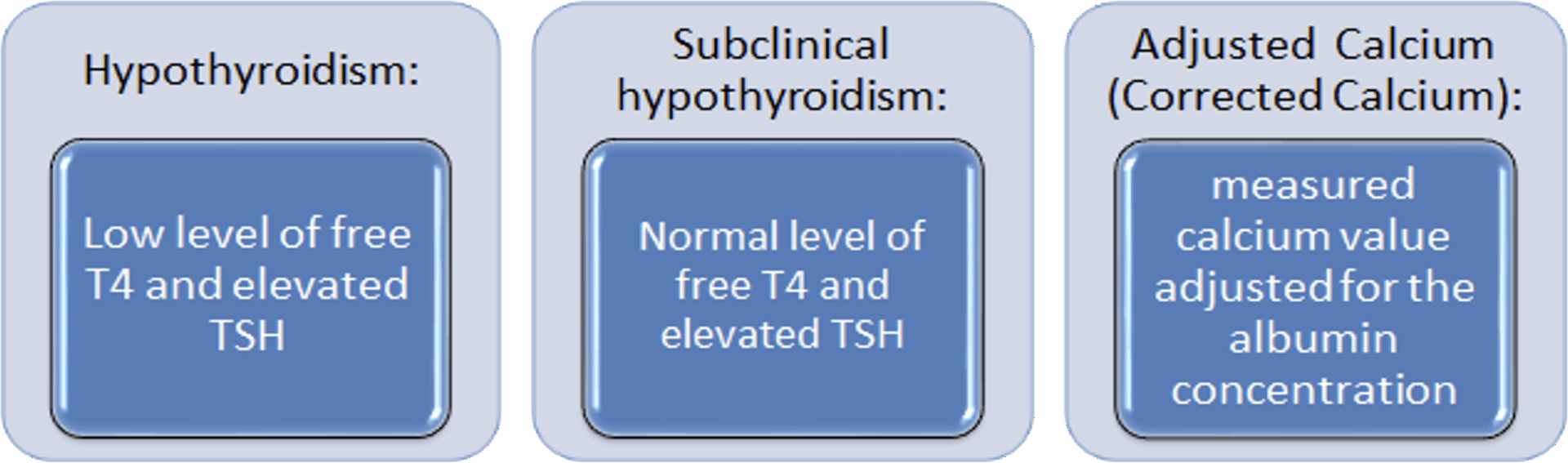
Hypothyroidism: Lithium has varied effects on Thyroid Hormone production and regulation, including inhibition of Iodine uptake in the Thyroid, inhibition of Thyroid Hormone synthesis and release, and hepatic conversion of free Thyroxine. Patient may present with typical hypothyroidism symptoms including lethargy, impaired cognition, weight gain, dry skin, and cold intolerance. Risk factors include females, older adults, family history of hypothyroidism, and presence of anti-thyroid antibodies.
Hyperparathyroidism and hypercalcaemia: Hypercalcaemia has been reported with Lithium therapy, which may or may not be related to drug-induced hyperparathyroidism. While lithium has been observed to affect Parathyroid Hormone levels after a single dose, long -term exposure is required to observe clinically relevant alterations in Calcium homeostasis.
Polydipsia and polyuria: Common adverse effects associated with lithium. Patients may notice increased urinary frequency (> 3 L in 24 hours) due to poor urine concentration; and increased thirst, which is independent of dry mouth effects of lithium.
Renal effects: Up to one-third of patients may develop some degree of decreased kidney function during the course of lithium therapy, with approximately 5 per cent developing significant kidney impairment/failure.
Sexual dysfunction: Studies report rates of the various effects of 5-40 per cent. Effects can include decreased libido, impaired sexual arousal, and erectile dysfunction. Sexual dysfunction can negatively impact a patient’s quality of life.
Tremor: Lithium can cause tremor in up to 25 per cent of patients, making it one of the most common adverse effects. This is commonly a bilateral, symmetrical hand tremor, which may spontaneously decrease over time as compensatory mechanisms develop within the patient. Course tremor and muscle twitching may be observed in lithium toxicity. Tremor commonly begins early in treatment, but can develop later in treatment, with or without a dose increase. Risk factors include higher doses/serum levels, medicines that can increase lithium level, medicines known to induce tremor (for example, antipsychotic, antidepressants), caffeine and older adults.
Weight gain: Increases of 4 to 7kg within the first year have been reported in the literature. Effects on central mechanisms related to weight gain, satiety and metabolism are possible. Increased consumption of high-calorie, sugary beverages from increased thirst with lithium could contribute.
Pharmacists should be aware of signs and symptoms of lithium toxicity.
For patients with symptoms of toxicity (for example, diarrhoea, vomiting, coarse tremor, mental state changes or falls), withhold lithium, refer to GP/Clinic/Hospital for urgent lithium level and U+Es, and seek specialist advice.
Referral to secondary care may be required depending on the severity of symptoms.
The national patient information booklet has been produced and updated by Audrey Purcell, Chief 2 Pharmacist and the Saint John of God University Hospital Drug and Therapeutics Committee. This initiative is intended to provide and promote safer lithium therapy and empower patients to engage with their healthcare professional to discuss all aspects of lithium therapy, monitoring, and side-effects. Appropriate information and monitoring are imperative to ensure best outcomes for patients on lithium therapy and reduce likelihood of harm.
The booklet has been reviewed and endorsed by Ciara Kirke, HSE Clinical Lead, National Medication Safety Programme. It has also been reviewed and endorsed by the Irish Medication Safety Network, Irish Pharmacy Union, and the College of Psychiatrists of Ireland.
It has also been edited and reviewed by the National Adult Literacy Agency and has successfully been awarded the plain English mark by NALA.
The Lithium booklet contains:
Pharmacists provide essential support and are recommended to:
National launch of the updated Lithium booklet, October 2025:
How to order national lithium booklets:
References available on request.
Acknowledgements: Many thanks to the following for article peer-review: Georgina Gilsenan, Senior Pharmacist, St John of God University Hospital; Margaret Brookes, Senior Pharmacist, St Patrick’s University Hospital, Sinéad McCool, Professional Services Pharmacist, IPU; and Ciara Kirke, HSE Clinical Lead, Medication Safety Programme.
Audrey Purcell B(Sc) Pharm

MPSI. MSc. Psych Pharm, Chief 2 Pharmacist, St John of God University Hospital, Stillorgan, Co Dublin, and Honorary Senior Clinical Lecturer, Royal College of Surgeons in Ireland.
Highlighted Articles