
The information provided was valid at the time of the publication of this CPD article.
Allergic rhinitis is the inflammation of the lining of the nose caused by allergens such as pollens, house dust mites, mould spores or animal dander. Allergic rhinitis is a common allergic disease with increasing prevalence; recent estimates suggest it affects over 30% of individuals, but not exclusively teenagers and young adults.

While considered by many as a trivial disease, allergic rhinitis, in addition to the nasal and ocular symptoms, can be irritating and when untreated, these symptoms can potentially impair patients’ ability to sleep and perform optimally in their daily professional or personal life. Children’s education is also particularly affected by untreated symptoms. It has been estimated that up to 90% of allergic rhinitis patients are untreated, insufficiently treated or inappropriately treated.
Pharmacists play an important role in the management and treatment of allergic rhinitis. They can advise patients on ways to minimise exposure to triggers, suggest suitable OTC treatment(s) and can recommend when the patient should see their GP.
The symptoms of allergic rhinitis include:
In severe cases, symptoms can interfere with daily activities and sleep causing fatigue and irritability. Also, it is common for asthma to coincide with allergic rhinitis; approximately three in four patients with asthma also suffer symptoms of rhinitis, which increases the risk of asthma attacks.
The symptoms of allergic rhinitis normally begin soon after exposure to the allergen. When rhinitis is caused by pollens or spores it is known as seasonal; symptoms will only occur in certain months and not all year round. For instance, grass pollens cause symptoms between May and September whilst most tree pollens cause symptoms between March and May. When rhinitis is caused by house dust mite allergens, it is classed as perennial; symptoms can occur all year round although they tend to peak in the winter.
As you can see from Figure 1, rhinitis can be classified as either intermittent (less than four days per week or less than four weeks duration) or persistent (greater than four days per week and greater than four weeks duration) and further classified as either mild or moderate to severe with more patients suffering the latter.

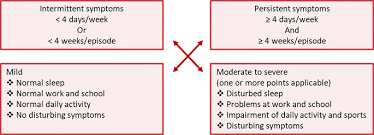
Figure 1: ARIA classification of allergic rhinitis
Allergic rhinitis results from an immunological abnormality in which atopic individuals produce antibodies immunoglobulin E (IgE) to allergens (e.g. pollen, house dust mites, animal dander and moulds). When allergens reach the nasal mucosa, the immune system is stimulated to produce IgE that will bind to and prime mast cells and other inflammatory cells. Also, the antigens located on the allergens interact with the mast cell IgE, causing it to release histamine to make the local environment hostile (e.g. producing mucus and stimulating sensory nerves to cause sneezing). Mast cells also produce cytokines to stimulate the influx of inflammatory cells, particularly eosinophils that contain several toxic proteins and cause local inflammation. Histamine stimulates the early symptoms, predominately mucus production, nasal itching and sneezing. Leukotrienes and cytokines attract and activate eosinophils to cause allergic inflammation, which is primarily responsible for nasal blockage.
Allergic reactions do not happen the first time someone comes into contact with an allergen. The immune system must recognise and memorise the allergen, a process known as sensitisation. The time taken to become sensitised to an allergen varies from days to years.
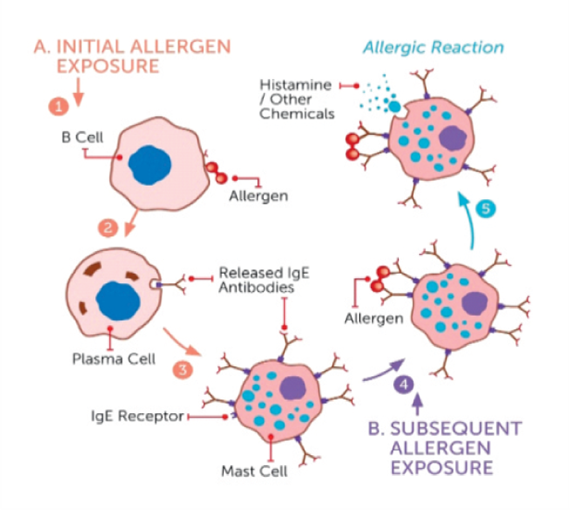
Figure 2: Allergen exposure immune response
Common allergens:
A child’s risk of allergy is as low as 5% where neither parent is affected by allergy. If both parents are affected by allergy, the risk rises to as high as 60% in some cases. People who are atopic are more likely to develop allergies because their bodies produce more IgE antibodies than normal. There is also an increased chance of a child developing atopic allergies growing up in a house with smokers, exposure to dust mites, exposure to pets and antibiotic use.
Complex cases, or cases where there may be an alternative diagnosis, should always be referred to a GP.
Also, it is advised that a patient is referred to a GP if allergic rhinitis is:
A diagnosis of allergic rhinitis is confirmed by allergy testing along with a detailed patient history and examination.
Skin prick test: This is usually the first test to be carried out when looking for an allergen. The skin is pricked with a tiny amount of the suspected allergen to see if there is a reaction. The testing is considered very safe and can be used on almost any age group. However, it may not be suitable if a patient has had a history of severe reaction to an allergen.
Blood test: This is used to measure the amount of IgE antibodies in the blood that have been produced by the immune system in response to a suspected allergen. The results are given on a scale from 0-6, with 0 indicating a negative result and 6 indicating an extremely high sensitivity.
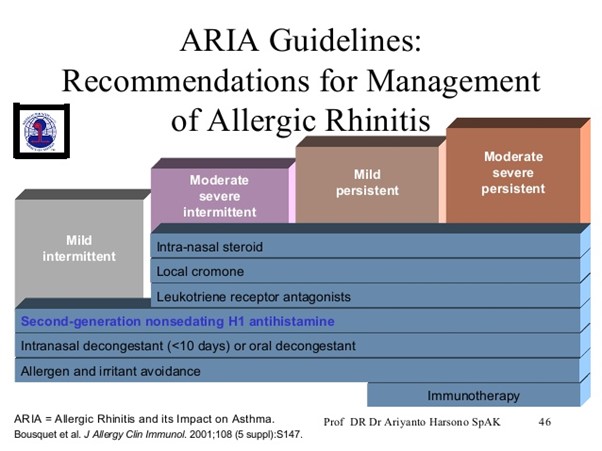
Second generation H1 antihistamines (e.g. loratadine, cetirizine) are effective as a single treatment in patients with mild to moderate forms of allergic rhinitis. They have a rapid onset of action and can be used as a rescue medicine to help alleviate the symptoms of the onset of acute allergic rhinitis. Although antihistamines demonstrate efficacy for the control of symptoms like sneezing, itching, rhinorrhoea or eye streaming, they are considered less effective than intranasal corticosteroids for treating nasal obstruction as corticosteroids have a much stronger anti-inflammatory effect.
Intranasal corticosteroids (e.g. beclomethasone, fluticasone) are the primary treatment for nasal obstruction. In both seasonal and perennial allergic rhinitis causing nasal obstruction, the ARIA guideline advises that intranasal steroids should be used as a first treatment option in adults. The theory behind this is that they act locally in the nasal passages, where the inflammation occurs, and high medication concentrations can be achieved at receptor sites. One thing to remember is the delayed onset of action for several days for intranasal corticosteroids.
Intranasal decongestants (e.g. xylometazoline) are asympathetic receptor stimulants and cause constriction of the arterial vessels delivering blood to the nasal capacitance vessels, therefore starving them of blood. They are briefly effective and rapidly acting but they may only be used for short periods (less than 10 days). If used for longer periods, rhinitis medicamentosa, a condition characterised by nasal congestion without rhinorrhoea or sneezing, may occur because of a reduction of blood vessel alpha adrenergic receptors. Patients should be counselled regarding this process.
Oral decongestants (e.g. pseudoephedrine) are weakly effective in reducing nasal obstruction but have a longer duration of up to six hours than nasal decongestants. Owing to their sympathomimetic effects, they should not be used by individuals with hypertension.
It is the only treatment that alters the disease course. It should only be considered when allergic rhinitis is debilitating and poorly controlled by pharmacotherapy. Subcutaneous immunotherapy is initiated by a specialist which involves allergen injections at regular time intervals (weekly or less) while the allergen doses are gradually increased. Therapy is for three consecutive years and can boost tolerance for up to 15 years. This type of treatment must be carried out under the close supervision of a doctor because there is a risk it may cause a serious allergic reaction. Sublingual immunotherapy is considered to be much safer. The initial dose is given under supervision but can be controlled on a daily basis at home.
Other options include topical cromone (e.g. sodium cromoglicate) when ocular symptoms are present and leukotriene receptor antagonists (e.g. montelukast) in the case of concurrent asthma.
If allergic rhinitis does not respond to single medicine treatment, add on treatments are then considered.
Nasal polyps can form as clusters on the lining of the nose and sinus cavities as a result of inflammation of the membranes associated with rhinitis. Polyps can interfere with breathing, affect sense of smell and contribute to sinusitis. Smaller polyps can be shrunk using corticosteroids. Larger polyps may need to be surgically removed.
Sinusitis is a common complication of rhinitis. The inflammation of the sinus mucosa generally creates favourable conditions for bacterial growth.
It is important to advise patients on the importance of the regular and correct use of their medicines to prevent complications of allergic rhinitis from developing. Allergy medicine works better if taken on a regular basis rather than ad hoc when symptoms are severe. Pharmacists should advise patients how to correctly administer their treatment as well as reviewing its effectiveness regularly.
The best way to prevent an allergic reaction is to avoid the allergen that causes it.
House dust mites
Pets
Pollen
References available on request
| Self-appraisal | What do you know about allergic rhinitis? What causes allergic rhinitis? What are the symptoms of allergic rhinitis? Do I see many cases presenting in pharmacy? What is the best advice to give patients with these symptoms? |
| Personal Plan Including a list of desired learning outcomes in a personal learning plan is a helpful self-analytical tool. | Create a list of desired learning outcomes. How will I accomplish these learning outcomes? Identify resources available to achieve learning outcomes. Develop a realistic timeframe for the plan. |
| Action Activities chosen should be outcomes based to meet learning objectives. | Implement plan. Read this article on allergic rhinitis. Consider the treatment options you are currently recommending and examine if you might be able to offer more effective advice. Review the OTC products you are currently recommending. Consider identifying and reviewing patients with allergic rhinitis. |
| Evaluate Consider outcomes of learning and impact of learning. | Have I met my desired learning outcomes? Do I now feel confident to engage with and counsel patients (and carers) about allergic rhinitis? Provide an example(s) of changes that I have implemented in my pharmacy practice. Have further learning needs been identified? |
| Document your learning | Create a record in my ePortfolio. As part of this record, complete an evaluation, noting whether learning outcomes were achieved and identifying any future learning needs. |
Grainne Doyle MPSI

Share This Page