- Public want expanded role for pharmacists; Government must listen
- Irish Pharmacy Union (IPU) conference hears pharmacists are willing and able to help address health service capacity problems
IPU, Sunday 29 April 2018: Pharmacists today called on the Department of Health to improve patient care and address serious problems in health service capacity by expanding the range of healthcare services pharmacies can offer.
The call was made at the Irish Pharmacy Union’s (IPU) National Pharmacy Conference and AGM, at which a motion was passed to introduce properly resourced pharmacy-based services. Pharmacists declared at the conference that they are ready, willing and more than capable of playing a greater role by expanding the services they provide and alleviating pressure on other areas in the health service.
Speaking to the motion, IPU President Daragh Connolly said, “There is a crisis in the health service and it is steadily getting worse. Government plans to reorient the health service towards primary care are leading to an over-reliance on GP services that GPs themselves have consistently argued is unsustainable. Government must look to address health service capacity challenges and improve patient care through the introduction of properly resourced pharmacy-based healthcare services.”
He continued:
“Population changes in the coming years will put further demands on an already overstretched health service. Pharmacists play a vital part in primary healthcare and are trusted by patients, but they are an underutilised resource.”
Community pharmacy is the most accessible part of the healthcare system, with 81% of people visiting a pharmacy at least once a month, according to research from Behaviour and Attitudes. The research also found that the public especially values pharmacies’ efficiency, opening hours, ease of access and lack of need for an appointment. 86% rate their pharmacy experience as good or very good and 74% of patients value the advice of their pharmacist.
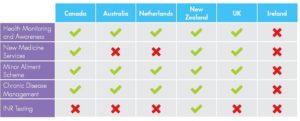
Ireland is currently far behind countries such as Canada and the UK, where community pharmacies are providing an increased range of services. These services include pharmacy-based Minor Ailment Schemes, provision of contraception and a wide range of vaccination services without the need for a doctor’s prescription, New Medicine Services, and management of chronic diseases such as hypertension. The experience in these countries has shown that involving pharmacies in this kind of healthcare has delivered significant benefits to both patients and the State, taking pressure off other parts of the healthcare system, including GPs and hospitals, and leading to better health outcomes. (see Table 1).
Research also shows that the public want more services from their local pharmacy. 96% of people surveyed said they “would be in favour of the pharmacist being able to prescribe some medicines for minor ailments”, while 93% said they would like to see the pharmacy “offering services such as blood pressure or cholesterol testing at the pharmacy for a reasonable cost”.
In conclusion Mr Connolly said:
“The focus of the healthcare system must be towards the creation of a patient-focused health service delivered at the lowest level of complexity and as close to people’s homes as possible. Pharmacists play a vital role in ensuring patient safety and wellbeing, and are available and willing to engage on a change agenda which involves expanding the role of the pharmacist and enhancing pharmacy services for the betterment of the healthcare system.”
ENDS
Further information: Jim Curran, IPU Director of Communications & Strategy, 086 264 0469
Siobhán Kane, IPU Press and Communications Manager, 087 7751510
Graham Union, MKC Communications, 086 7790744
Notes to Editors:
Table 1: Examples of Community Pharmacy Services in other countries
What is the Minor Ailment Scheme?
The primary aim of a Minor Ailment Scheme is to enable medical card patients to receive treatment for common illnesses free of charge directly from their local community pharmacy in a timely manner and without the need for a visit to the GP. At present, private patients who want to access non-prescription medicines for ailments such as hay fever, migraine or skin conditions, consult with their local pharmacist on the best option for them, and pay for their over the counter medication. Medical card patients with the same ailments can only access the same medicines if they visit their GP and get a prescription. If a Minor Ailment Scheme were introduced, public patients would no longer have to make and wait for GP appointments, saving time for both GP and patient.
18% of a GP’s workload is spent dealing with minor ailments. At a time when GPs are already overworked and we face a GP manpower crisis, the scheme could save nearly 950,000 unnecessary GP consultations every year, freeing up the equivalent of an additional 91 full time GPs and, in the process, keeping the focus on primary healthcare in the community. The IPU has already collaborated with the Department and the HSE on a pilot scheme, and the final report was forwarded to the Department and HSE in June 2017.
What is the New Medicine Service?
A New Medicine Service can improve adherence to medicines for people who have been newly prescribed medicines for certain long-term conditions or therapies such as asthma, COPD, Type 2 diabetes, hypertension, antiplatelet/anticoagulant therapy, statin therapy and chronic pain. The service, would require a structured pharmacist-led intervention, delivered within the community pharmacy setting, consisting of advice and support for patients prescribed medicines for a specific chronic disease.
Economic analysis of a similar service which has operated in the UK since 2011 found that it offers the NHS increased health gain at reduced overall cost, and provides short-term savings of £75.4 million and long-term savings of £517.6 million. A successful Pilot has been completed here in Ireland, which identified a 9% improvement in adherence and a report has been submitted to the Department of Health.
What is the Blood Pressure Management Service?
The clinical benefits of pharmacy involvement in chronic disease management are compelling, with a large evidence base detailing that pharmacists have the most frequent contact with patients with chronic diseases due to their accessibility and that pharmacists could provide clinical and cost benefits through the existing community pharmacy network. It is envisaged that chronic disease management will be a collaborative initiative between the GP, practice nurse, community pharmacist and other healthcare providers. A pharmacist led blood pressure (BP) management service could potentially lead to 71,600 cardiovascular events being avoided in the Irish population and an estimated saving of €1.36 billion over a 30 year period.
How can pharmacists help improve women’s access to contraception?
The IPU proposes that the Department of Health and the HSE put in place a scheme to enable women to access contraception directly from their community pharmacist without prescription and without charge, regardless of eligibility. In March 2018 Minister for Health Simon Harris proposed to introduce a free contraceptive scheme, and the IPU has provided a submission outlining the important role pharmacists can play in improving women’s access to contraception.
Pharmacists have directly provided emergency contraception without the need for a prescription since 2011, and most women now obtain emergency contraception from pharmacies rather than from GPs. This reinforces findings from a 2010 HSE study on contraception and crisis pregnancy, which found that convenience and accessibility are important for the supply of contraception. The same study showed that nearly half of the women surveyed (47%) reported that they would prefer to get their contraception from a pharmacy. The IPU proposal would ensure equity and convenience for women seeking to access contraception, and would increase patient safety by ensuring women getting contraception see a trained medical professional rather than relying on online resources.